CMS’ 2026 proposed rule introduces changes for ACO quality reporting
At a glance:
A new care model, updated reporting requirements, and shifting incentives are reshaping how ACOs must approach CMS quality reporting in 2025 and beyond.
In a recent webinar with Arcadia partner Medisolv, we explored key takeaways from CMS’ 2026 proposed rule, including changes to ACO quality reporting requirements. The discussion also covered the new mandatory Ambulatory Specialty Model (ASM) and immediate steps ACO leaders should take to prepare.
The Centers for Medicare and Medicaid Services (CMS) released a proposed rule that would implement changes to the physician fee schedule, effective in calendar year 2026. As CMS stated in its news release, “the proposed rule is one of several proposed rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better quality, efficiency, empowerment, and innovation for all Medicare beneficiaries.”
While the agency solicits feedback on its proposed rulemaking, Accountable Care Organizations (ACOs) are closely watching how CMS plans to approach quality reporting in 2025 and beyond. In short, leaders should expect updated reporting requirements and shifting incentives. In this article, we’ll break down what you need to know.
New model for specialists
Among the most significant elements of CMS’ proposed rule is the introduction of a new mandatory payment model: the Ambulatory Specialty Model (ASM). Designed to shift more accountability onto outpatient specialists, ASM will have direct implications for quality performance, data aggregation, and care coordination.
The ASM aims to improve outcomes for patients with chronic conditions by implementing upstream disease management and enhancing coordination. Initially, it will target cardiologists treating heart failure and specialists treating low back pain, including anesthesiology, interventional pain management, neurosurgery, orthopedic surgery, pain management, and physical medicine and rehabilitation.
CMS will release a list of selected participants by the end of 2025 with a finalized list release by July of 2026. ASM participants are mandated to participate in the model.
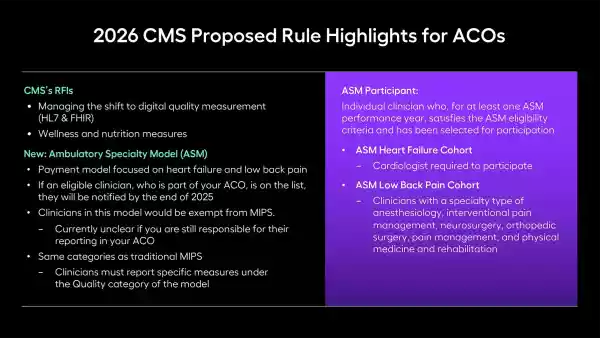
While eligible clinicians would be exempt from the merit-based incentive payment system (MIPS), it’s currently unclear whether ACOs would still be responsible for reporting ASM-eligible clinicians. CMS specified in their ruling that ASM was designed to interact with other models. So, a clinician in an MSSP ACO could also be an ASM participant. It’s not yet clear whether ACOs must still report for those ASM participants. Further clarity is expected when the final rule is released later this year.
In the meantime, ACO leaders with multispecialty participation should begin scenario planning now—especially if your organization includes cardiologists or musculoskeletal specialists—so you can adapt to potential changes in attribution or data handoffs.

The model raises unresolved questions for ACOs. For example, if an ASM-participating specialist is also part of an ACO, will the ACO remain responsible for reporting quality data on their behalf? CMS has not clarified whether ACOs would be exempt from including these clinicians in their reporting submissions.
Key updates from CMS’ 2026 proposed rule
Beyond ASM, the proposed rule includes a suite of updates that together signal a significant evolution in how CMS expects ACOs to report and perform. Most notably, the proposal did not resurrect the CMS Web Interface measures, meaning it is still not available as a reporting option in 2025. While its demise is largely anticipated, this is a nail in the coffin. Instead, ACOs must use one of three other measure collection types in 2025: eCQMs, CQMs, or Medicare CQMs. Note that CQMs are only available for the 2025 and 2026 reporting years.
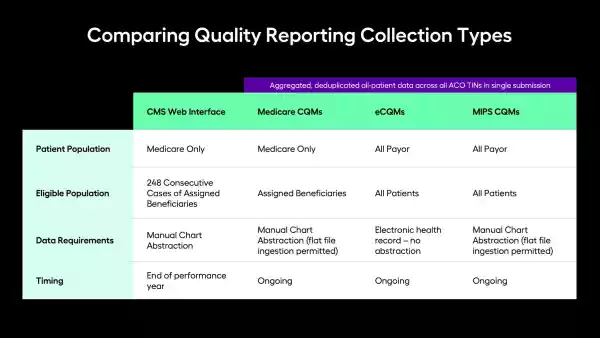
One thing that would not change is incentives for electronic clinical quality measure (eCQM) and MIPS clinical quality measure (CQM) reporting, meaning ACOs that submit via these methods can still qualify for reporting incentives and a bonus “complex organization adjustment” point per eCQM.
Health equity and SDoH
CMS proposed eliminating the social drivers of health (SDoH) screening measure requirement planned for implementation in 2028. CMS also proposed removing the health equity benchmark adjustment (HEBA). Notably, CMS did include the SDoH screening measure in the ASM program as an Improvement Activity measure. In this instance, the specialist doesn’t need to perform the screening themselves, but instead, coordinate with the beneficiary’s primary care physician (PCP) and confirm the PCP completed the screening. This could be an early indication from CMS of what they intend to do to incorporate these screening questions back into these programs.
Other changes of note
Under the proposed rule, CMS would expand the administration of Consumer Assessment of Healthcare Providers and Systems (CAHPS) to web, mail, and phone by plan year 2027. CMS would also expand the criteria for its emergency exception policy to include cyberattacks as an “extreme and uncontrollable circumstance.”
Additional elements of CMS’ proposal that ACO leaders should consider are change of ownership (CHOW) reporting requirements, which would require ACOs to update their participant lists when an ACO participant or an ACO’s skilled nursing facility (SNF) affiliate experiences a CHOW. CMS also intends to revise the definition of an eligible beneficiary for the Medicare CQM measure collection type only. They propose it will now be defined as “had at least one primary care service with a date of service during the performance year. CMS will include an additional flag on quarterly list, “beneficiaries eligible for Medicare CQMs.” This flag indicates the patient had a primary care service visit, and will be included starting with the Q2 2025 quarterly file.
Future of quality reporting
The proposed rulemaking reinforces CMS’ direction: greater accountability for specialists, more robust digital infrastructure, and strategic incentives to accelerate performance improvement. ACOs that act now to modernize reporting workflows and align with the eCQM ecosystem will be best positioned to meet the evolving requirements and retain shared savings.
