Adequate hospice care reduces end-of-life costs and utilization
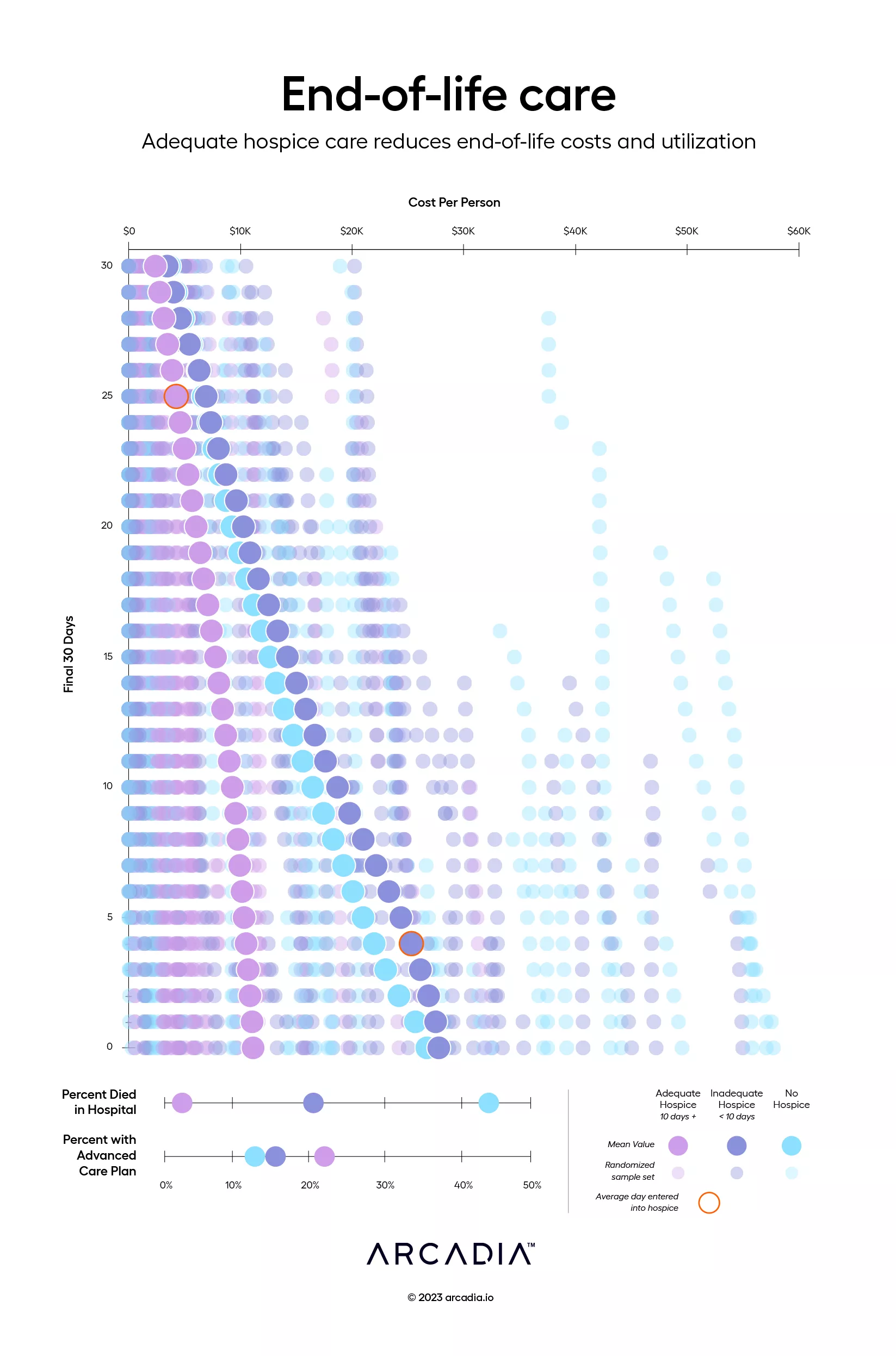
The final thirty days of a person’s life are arguably the most important. Adequate hospice care gives patients and their families the dignity they deserve during this time and contributes to reductions in unnecessary utilization and medical costs.
This visualization is a snapshot of Medicare patients who have passed away, divided into three categories: those without enrollment in hospice care, those with less than ten days of end-of-life care (inadequate hospice), and those with at least ten days of care prior to death (adequate hospice). The average cost of care for each category is represented by the trend line made up of solid dots. Those who are enrolled in an adequate amount of hospice see marginally increasing costs each day leading up to their death, whereas patients with no hospice tend to see costs spiral out of control. Patients with inadequate hospice also see a sharp increase in costs, though these typically begin to stabilize in the final few days.
The two charts at the bottom show that patients who had an advance care plan in place prior to their final month of life were more likely to be enrolled in hospice at least 10 days prior to death, and subsequently far less likely to die in the hospital. This suggests that these patients may also experience a more comfortable, higher quality end-of-life experience.
Details
D3.js, Excel, and Illustrator
Data sourced from Arcadia’s Medicare ACO population using claims and clinical surveys
