Data on FHIR: Interoperability standards for whole-person care
FHIR (Fast Healthcare Interoperability Resources) opens up pipelines to deliver data from disparate sources to providers to enable whole-person care. But, FHIR alone isn’t enough to bring together a whole picture for the patient. In Arcadia’s Byte-Sized Insights, Brendan Smith-Elion, VP of Product Management at Arcadia, explains the challenges healthcare organizations have with getting across the finish line with FHIR and how they can get the best results out of interoperability standards.
Four roadblocks to enabling whole-person care
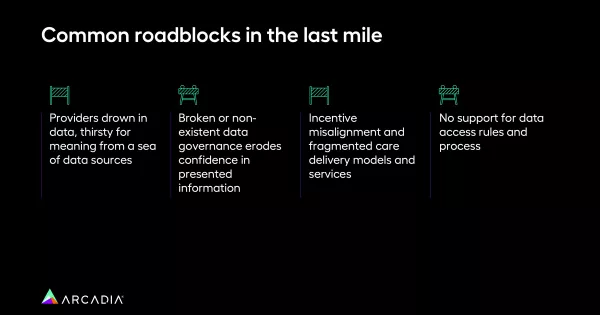
Smith-Elion says, with FHIR, we have the ability to access a huge data set across a variety of sources, but we need to make sense of that data. He outlines four main roadblocks to enabling whole-person use cases:
- Drowning in data: Pulling in every type of data on a particular issue, such as allergies, is overwhelming because there is no intelligent deduplication or inherent logic to make sense of it all.
- Broken or non-existent data governance: Without alignment between the content coming through FHIR and the use cases the healthcare organization wants to enable, providers lose confidence in the information.
- Incentive misalignment: Healthcare organizations must understand why this data will change a provider’s mind or encourage an action and align it with the care models.
- No support for data access rules and process: A third-party system is required to give providers with the right detailed access.
“Today we’re still misaligned between incentives. We’re still in a fragmented state where FHIR endpoints are sending a whole swath of data, streaming all this information out, but it’s not actually aligned with what that end use case is,” said Smith-Elion. “We need to push for a comprehensive data fabric; a well-designed, well-aligned solution with the teams and the use cases that we’re trying to push.”
Creating value from FHIR requires more than compliance
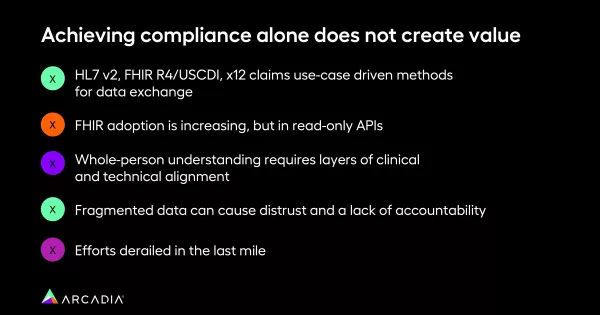
The rules and regulations today enable FHIR. However, compliance alone will not drive meaning, deduplicate, or ultimately create value from the data. To be successful, there are several potential obstacles healthcare organizations need to have on their radars:
- While overall FHIR adoption is increasing, the increase is limited to read-only APIs (pulling data out of an EHR system). Adoption of write-back FHIR APIs (sending data back into the system) is still minimal.
- Whole-person care requires alignment between both the technical and clinical perspectives.
- Fragmented data can cause distrust and lack of accountability.
- Only considering one piece of technology or one specific use case (not considering the full tech stack) can derail FHIR at the last mile.
“It can actually erode trust if you’re just shooting data to the provider at the point of care and cause accountability issues,” cautioned Smith-Elion.
Example: Blood pressure data
Blood pressure is a great example of just how complicated it can be to drive meaning from the data. Knowing the blood pressure reading is not enough. You also need to know how the data was collected, how the blood pressure was collected from the patient, and the timing of the collection to bring meaning to the data.
“FHIR allows us to access all this data, but you have to contextualize it. You have to have the data around it to provide meaning,” said Smith-Elion.
There are 163 ways of representing blood pressure. It is important to ensure that you do not exclude data points that would be relevant. Therefore, you need to have a terminology service in your solution to map it to the right code.
Trust in the data among providers is also critically important. Trust is built by allowing them to see the surrounding data and ensuring the source is appropriate and clinically accurate.
Building an integration strategy
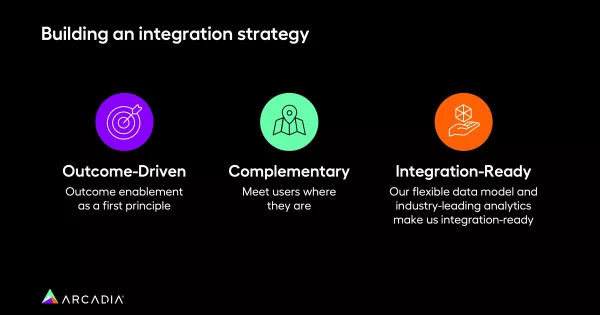
Simply opening up FHIR will not get you very far in enabling whole-person care. Think about the outcomes and end use cases you would like to achieve and build backwards from there. Future proof your work by building flexibility into the models. Watch more Byte-Sized Insights or request a demo to learn how we can put your data to work, together.
