How an ACO revolutionized high-risk maternity care with data-driven strategies
In 2023, Massachusetts Medicaid (MassHealth) rolled out a new Accountable Care Organization (ACO) waiver, sparking the creation of a high-risk maternity program. This program is essential for supporting Medicaid recipients, offering comprehensive care from pregnancy through 12 months postpartum.
Simply put, women with high-risk pregnancies need better care. Medicaid patients, in particular, have complex medical, behavioral, and social needs. Let’s dive into how Community Care Cooperative's implementation started, its early successes, and how data analytics brought it all to life.
Tackling high-risk maternity care
Addressing health disparities in vulnerable populations is crucial, particularly in high-risk maternity care. Pregnancies with risk factors need targeted interventions to improve outcomes. These risk factors include severe behavioral health issues, substance use, chronic diseases, food insecurity, and housing insecurity.
Accountable Care Organizations (ACOs) play a key role in Medicaid, enabling coordinated care that improves patient outcomes and cuts costs. By bringing healthcare providers together, ACOs aim to enhance care quality while managing costs effectively.
When the 2023 MassHealth ACO waiver mandated the creation of a high-risk maternity program, Community Care Cooperative stepped up to the plate. With 215,000 lives covered under MassHealth, it was essential for Community Care Cooperative to establish a structured program to support high-risk pregnancies.
Data-driven approach to high-risk maternity care
The mission was clear: develop a program capable of identifying and supporting high-risk maternity patients. This required not only meeting state requirements but also meet state requirements and address the needs of its target population. The program supports members from pregnancy through 12 months postpartum, a significant shift from Community Care Cooperative’s short-term care management programs.
Methodology and race, ethnicity, and language (REL) data
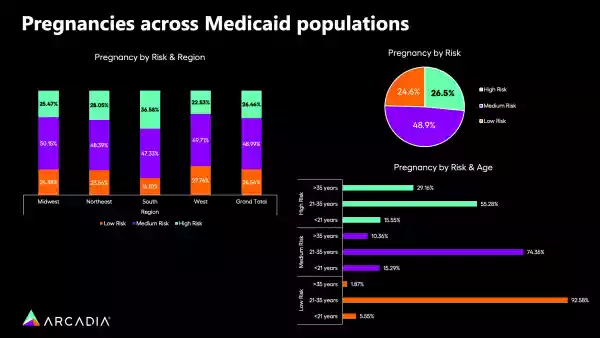
The program's data-driven approach incorporated a wide range of risk factors, both prescribed by MassHealth and recommended by Arcadia. These included medical, behavioral, and social determinants of health (SDoH). Key risk factors were:
- Previous pregnancy complications
- Severe behavioral health issues
- Substance use
- Chronic diseases (e.g., chronic kidney disease, diabetes, HIV)
- Food insecurity
- Housing insecurity
- Race
MassHealth's definition of high-risk pregnancies includes not only medical complexities but also behavioral and social drivers of health. This broader definition required Community Care Cooperative and Arcadia to consider a wide range of risk factors and data sources to shape the program’s framework and close risk gaps at the point of care.

Arcadia brought a wealth of experience and innovative solutions to the table. Their understanding of social determinants of health and data-driven approach helped us design a comprehensive and effective program.
Integrating data sources for high-risk maternity care
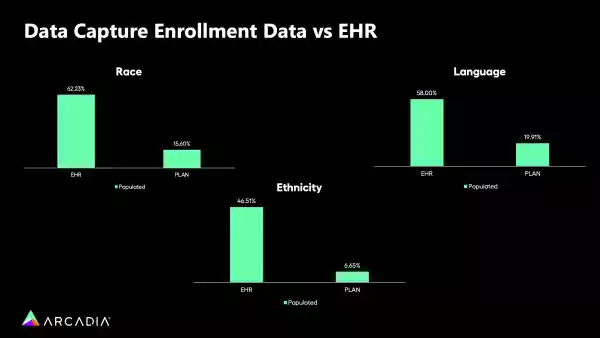
Community Care Cooperative and Arcadia gathered data through several methods:
- EHR connectors: Linking electronic health records (EHR) from all Massachusetts health centers to Arcadia's platform.
- Annual SDoH screenings: Conducted for all members to assess social determinants of health.
- Care management assessments: Performed by care managers during regular assessments.
Arcadia's platform aggregated and analyzed this data to identify high-risk members effectively.
Our partnership with Arcadia enabled us to bring together data from multiple sources, giving us a comprehensive view of our members' needs. This holistic approach was essential for identifying high-risk individuals and providing targeted interventions.
Building the high-risk maternity program
The program features both centralized and decentralized care management teams. Centralized teams supported health centers lacking internal resources, while decentralized teams use Arcadia's data to manage the program independently.
The teams included:
- Maternal health care managers: Nurses specializing in maternal health.
- Doulas: Providing support during and after pregnancy.
- Lactation consultants: Assisting with breastfeeding and newborn care.
Community Care Cooperative’s program structure provided tailored support to each health center. Some health centers have their own care managers who use Arcadia's data to manage the program, while others rely on centralized teams for support. This flexible structure ensured that all members received the care they needed, regardless of their health center’s resources.
Effective interventions and resources for high-risk maternity
Community Care Cooperative’s tailored interventions to address identified risk factors. These included:
- Clinical assessments: Comprehensive medical and behavioral health evaluations.
- Care plans: Personalized plans with goals and interventions.
- Behavioral health support: Including postpartum depression screenings up to 12 months postpartum.
- Nutritional and housing assistance: Connecting members to programs like Community Servings & Project Bread for nutritional support and housing assistance.
The high-risk maternity program was designed to address questions about issues like food insecurity when tangible support could be provided. This approach ensured that interventions were both effective and meaningful.
Transformative maternal health: 5 positive impacts on high-risk members
Member enrollment impact
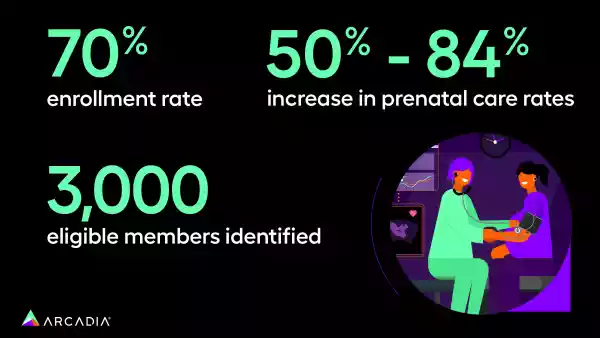
In its first year, the program identified over 3,000 eligible members, with more than 1,000 enrolling — achieving an impressive enrollment rate of approximately 70%. This success highlights the program's effectiveness in engaging high-risk members and ensuring they get the care they needed.
Quality measures improvement
The program significantly boosted quality measures, particularly in prenatal and postpartum visit rates. One health center reported an increase in prenatal care rates from 50% to 84% after the program's rollout. This improvement shows the program's impact on healthcare outcomes and its ability to overcome barriers to care.
Visit rates and post-partum benefits
By identifying and addressing barriers such as transportation and childcare, Community Care Cooperative has significantly increased prenatal care visit rates. This is a critical factor in improving maternal and newborn health outcomes.
The program also focused on postpartum depression screenings, conducting them up to 12 months postpartum. This extended support period ensured that new mothers received the necessary behavioral health resources.
Community services and holistic care
The program also connected members to essential services, like nutritional support and housing assistance, through partnerships like Project Bread.
These collaborations enabled Community Care Cooperative to provide comprehensive support to their members. This holistic approach is essential for addressing the complex needs of high-risk maternity patients.
Future outlook for high-risk maternity programs
By leveraging data analytics and comprehensive care strategies, the high-risk maternity program shows the potential of innovative healthcare solutions to transform patient care and improve outcomes. With ongoing data analysis and intervention adjustments, the high-risk maternity program is well-positioned to further improve maternal and newborn health outcomes, providing a valuable model for similar initiatives nationwide.

We're excited about the future and the positive impact we're making on maternal and newborn health.
The success of this program would not have been possible without the dedication and expertise of the Community Care Cooperative team and the support of community organizations. Their collective efforts have set a new standard for high-risk maternity care and demonstrated the impact of data-driven, collaborative approaches in healthcare.
Learn more about how Arcadia can help you further advance care programs and improve health equity.
