Scaling Smarter: How Leading Health Plans Use Data to Improve Outcomes and Control Costs
New survey insights from Arcadia and Healthcare Dive reveal what separates high-performing health plans from the rest and how to apply their data strategies across your organization.

What’s inside:
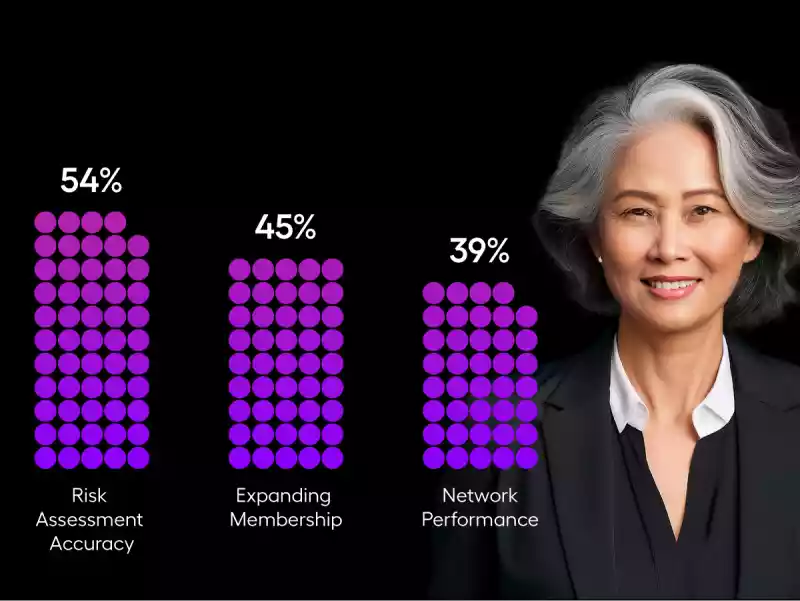
Payer priorities are changing with the market
Cost-containment now outweighs growth as a strategic priority, with most payers focusing on improving risk accuracy and network performance over expanding membership.
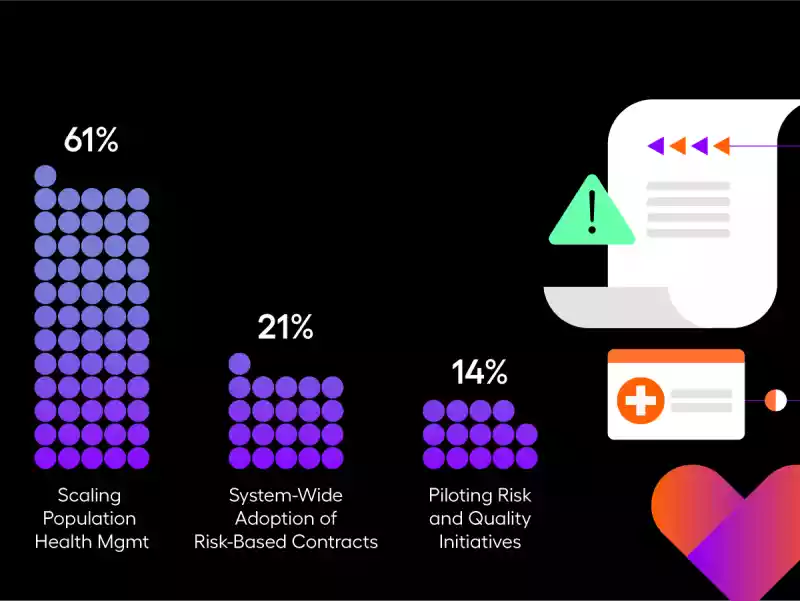
Growth Has Plateaued—But Performance Gains Haven’t
Policy changes and payment reform are making it more challenging to grow the bottom line. With little more to squeeze out of the sponge, plans — regardless of their participation in risk-sharing agreements — are turning to smarter analytics to drive better financial performance.
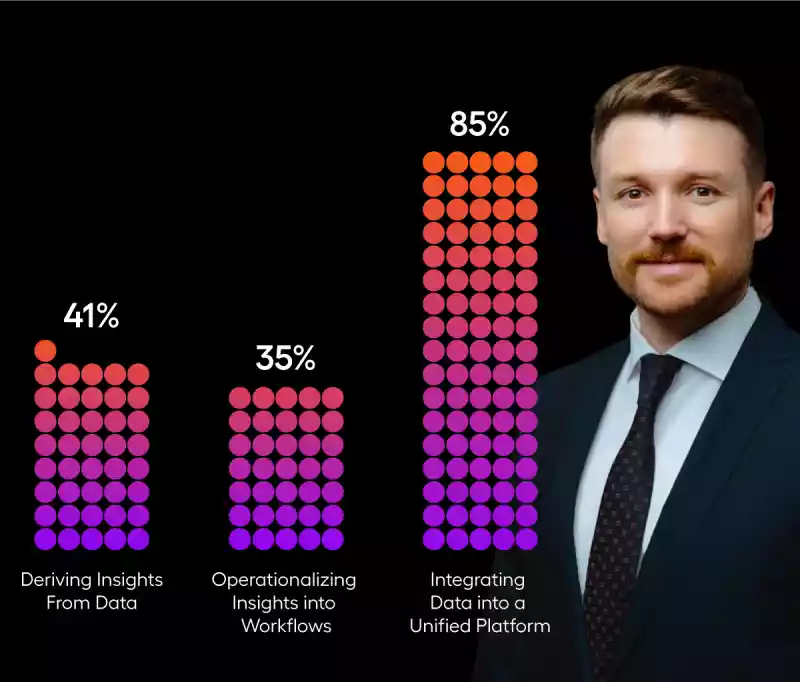
Everyone Has Data. Few Know What to Do With It.
Despite payers investing in analytics capabilities, fundamental challenges, like acting on insights, prevent some organizations from making the best use of technology.
Health plans that empower providers with data and tools create a competitive advantage, like closing more care gaps faster and improving outcomes at scale.

Improve your plan's performance
Download the report to learn how the most successful payer organizations are:
- Using longitudinal member data to improve accuracy and insight
- Driving quality and cost improvements through AI and analytics
- Enabling networks and providers to deliver whole-person care
Get the report
Fill out the form to access the full report and learn how to drive digital transformation in healthcare.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
