Care management, not IT, is your #1 focus
You need a platform that’s easy to use for analysts, providers, and executives so you can focus on the work that really matters: providing care to your patients. Top healthcare organizations partner with Arcadia to streamline workflows, leverage easy-to-use dashboards, and increase data visibility to enable better care for all.
Ready to put your data to work?
Let’s schedule a meeting to discuss how we can work together to create a trustworthy data asset to improving care management.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Join healthcare changemakers:




Clinical patient records
Best in KLAS winner for value-based care managed services
Claims and EHRs connected
In healthcare costs
Automate work distribution based on specific population needs and characteristics
Our workflow automation engine can be leveraged to automatically assign patients to specific care managers or specific program queues.
Reporting and business intelligence at your fingertips
Arcadia’s operational and performance insights give your users the information they need to benchmark and perform in value-based care to grow your network.
Patient and population health data you can tap into
Arcadia has deidentified population health trend data you can tap into and apply to your populations, including data assets from Massachusetts to Delaware to California.
Make the most out of patient engagements
We’ve partnered with Artera to increase patient engagement through two-way text, as well as one-to-many outreach campaigns with just a few clicks.

Enable your providers to perform under value-based care
Whether you have 100K or 1M managed lives, you need a platform that stays ahead of the curve and grows with you as you attract more providers to your network. Arcadia ACOs on average get $2M more in shared savings and $1M more in bonuses under value-based contracts.
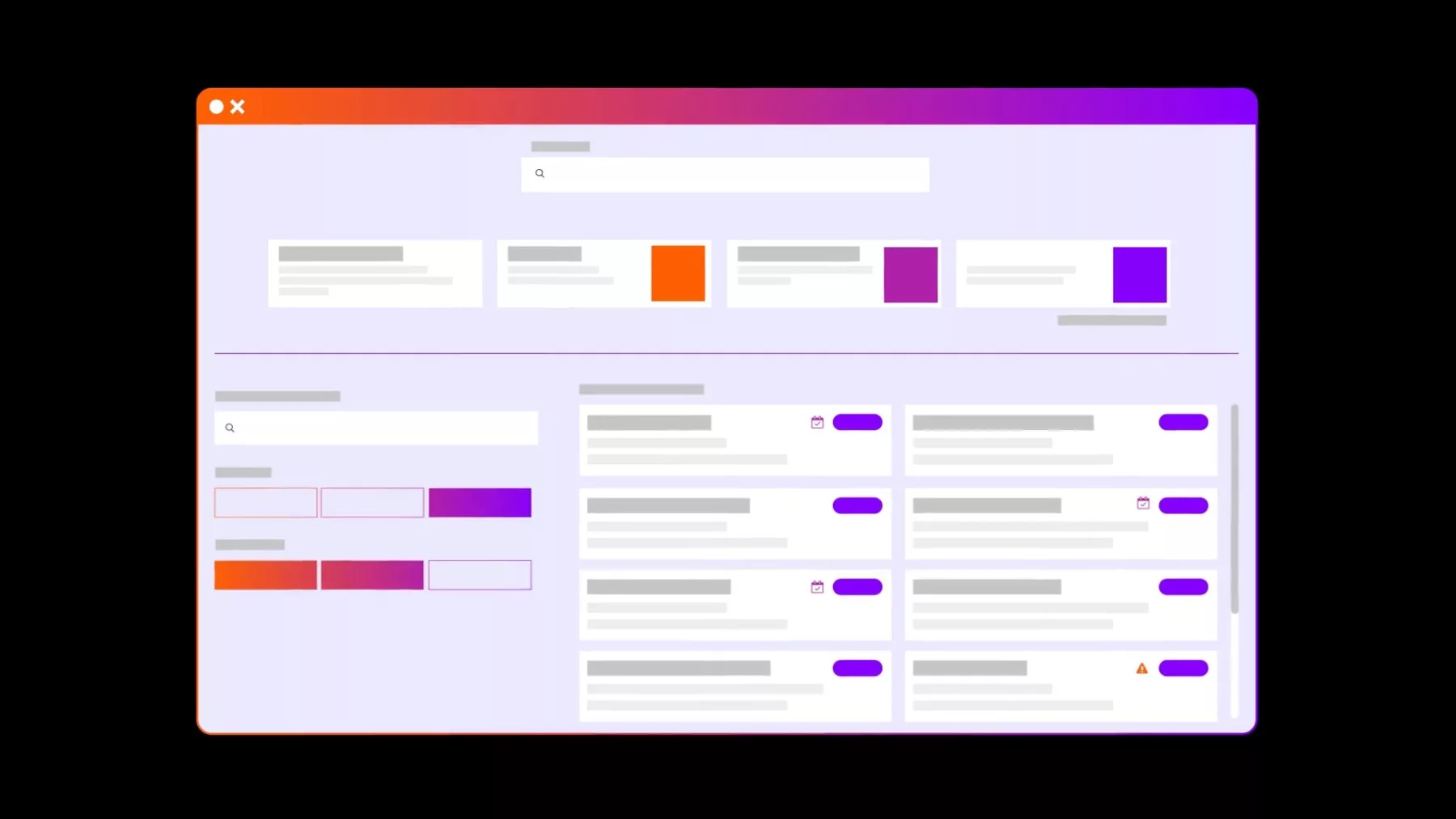
Narrow down a population of focus through risk ranking
Filter risk scores and other patient parameters as criteria to drive automated patient identification for care management programs and case recommendations.
Link patient records across data sources
Arcadia’s Master Patient Index (MPI) engine links together EHR-based patient data and payer-based member data using a series of algorithms that maximize data links while minimizing false-positive alignment.
Create and manage cohorts
Arcadia’s Population Explorer displays a tabular patient list with relevant demographics, utilization, and clinical data to narrow search and segment populations for specific use cases to close quality gaps.
Leverage clinical and claims data for case enrollment
With more than 50 identification triggers, including clinical events, patient demographics, patient attribution, and risk indicators, care teams can keep lower-acuity patients engaged in preventative care.
We use Arcadia Analytics not only for our analytics platform but also for our care management services and MSO. Other companies don't necessarily offer those things. So we would most likely stick with Arcadia if we made the same decision today. There is a lot of content in the product. We can use it for a lot of different functions, and it helps us drive performance and other things.
Ready to put your data to work?
Let’s schedule a meeting to discuss how we can work together to create a trustworthy data asset to improving care management.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
