Improve patient outcomes through better end-of-life care
End-of-life care. Not an easy subject.
Patients who pass away at hospice have a better transition than patients who pass away at home or pass away in the ICU. So it’s better for patients and much less expensive.
The greatest opportunity for your ACO
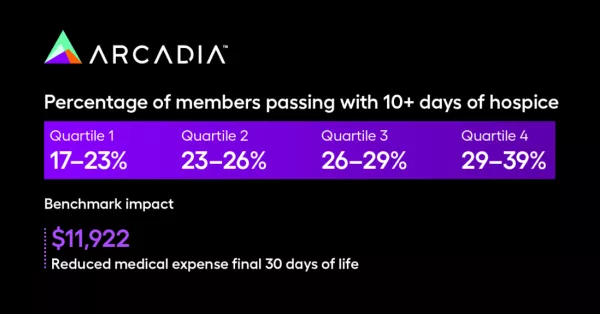
There’s a well-established opportunity to deliver better quality care to patients and improve MSSP results for your ACO. You can see in the benchmark below, created from Arcadia ACO customer data, that a small improvement in the % of members who passed away within an ACO who had 10+ days of hospice care prior to passing made a huge impact on cost.
It’s also a moveable metric. The simple fact is that you can get more of your eligible patients enrolled in hospice care with better education.
So why aren’t more ACOs dedicating resources to end-of-life care?
A sore subject
Jake Hochberg, Arcadia Executive Director of Customer Insights, says that the primary challenge is that end-of-life care is simply that it’s a sensitive subject.
“A lot of people don’t know how to run a program like this. They aren’t sure how to approach a patient to talk about end-of-life care,” says Hochberg.
It’s not as easy as going through lists of patients who are going to pass away and cold-calling them. This conversation must come from the PCP. That means that ACOs must identify eligible members early in the process and ensure their primary care physicians are well-educated on how to manage these conversations.
Additionally, ACOs must follow up with PCPs to ensure they’re doing that work.
Building a highly impactful end-of-life program
Hochberg says there are really three things Arcadia’s ACO customers are doing to ensure success in end-of-life care:
- They hire EOL positions and focus on end-of-life care education
- They use the data they have to identify patients nearing end of life
- They ensure physicians are following through with patients on end-of-life care
Success in this area is all about ensuring a patient that is sick, and is either hospice eligible or on the way to being hospice eligible, is coming into the office for an end-of-life care conversation. It’s also crucial that these patients have advanced care plans on file, so that when they’re ready to transition to hospice care, that conversation has already happened.
ACOs with access to Arcadia’s tools, says Hochberg, have a leg up on identifying eligible patients, tracking performance at the provider level, and performing outcomes analysis to justify investment.
A framework for better end-of-life care
Dr. Rich Parker, Arcadia Chief Medical Director, has additional insights for ACOs establishing effective end-of-life care programs.
Since 1985, Dr. Parker has felt strongly that when patients were coming down the home stretch, that was a really important time for their doctor to be involved with them and their family and help them navigate the end of life as peacefully as possible and in the way that they wanted. He published his career findings as an article in the Annals of Internal Medicine, entitled Caring for Patients at the End of Life.
“It turns out,” Dr. Parker says, “most people don’t want to die in a hospital. They don’t want to die on a ventilator in an ICU. They would rather be at home with their family and having the hospice nurse or doctor combined care for them.”
Most people don’t want to die in a hospital
To make this happen, ACOs have to drive initiatives from the top and make end-of-life a priority. Quality end-of-life care must be prioritized by Chief Medical Officers. It’s actually very simple:
- The Chief Medical Officer at the ACO must do their research, understand that better care is less expensive, and make the decision to invest in end-of-life care.
- The CMO must then bring the initiative to the CFO and CEO, define a budget, and make a business plan (Arcadia can help with this process).
- They must also hire a palliative care physician to oversee the initiative, which might require a half FTE plus some admin time.
- Once agreed, they need a strategy to roll it out — something ACOs are already very good at.
High-functioning ACOs typically have what Dr. Parker calls a “distributed leadership model,” where initiatives are driven from the executive level, but implemented by local leaders.
“A CEO and the chief medical officer can’t run a network of 1000 doctors, it’s not possible,” says Dr. Parker. “There’s something that I learned a long time ago called the square root rule. It states that for whatever number of doctors you have, that’s the number of leaders you need. So let’s say we have 900 doctors. We know the square root of 900 is 30. So you need 30 local leaders in your community, who will pick up this end-of-life care initiative, learn how to do it, explain it to their colleagues, find the time to teach them, roll it out, support it, get the data from Arcadia, and ensure its success.”
At the end of the process is a feedback loop. ACOs must measure, see how their PCPs are doing, then remeasure.
The goal is to see who is doing great, who’s not, and formulate a plan for improving those who are lagging behind. Here it comes full circle, because this is the work of the Chief Medical Officer with the support of their data team and care managers to research benchmarks and ensure overall success of the program.
“We have tools to compare all our customers and how they’re doing in end-of-life care,” says Dr. Parker. “It’s very powerful to show that to a leadership team and say, well, here’s where you stand relative to other customers, would you like to be at the top of the heap instead of the middle or the bottom?”
The myth of end-of-life care
There are two common myths around end-of-life care. First, that these conversations are difficult. Second, that they take a lot of time.
According to Dr. Parker, these are simply not true. In reality the conversation can take 10-15 minutes and is something that is probably on the patient’s mind already.
“The internist or the family practitioner, who maybe has cared for this patient for a decade or more, simply brings it up and says, ‘Today, I’d like to have an important conversation with you, as you may be coming towards the end of your life, about what your wishes would be.’“
So what’s holding most physicians back?
Education leads to better outcomes
ACOs who invest in education and incentivize their physicians to participate end up sharing in the savings from better end-of-life care outcomes. All it takes is a few hours of education. Dr. Parker also recommends offering physicians CME credits for their participation or even paying them for their time.
“There are different ways to do it. But it’s got to be a priority. Because everyone’s bandwidth limited, there are only so many things you can ask doctors to do. And if this has got to be one of them, then you’ve got to do it efficiently. And then you’ve got to measure it, and give them the feedback on how they’re doing.”
When Dr. Parker worked at Beth Israel Deaconess as the Chief Medical Officer, one of his primary Medicare initiatives was end-of-life care. For the end-of-life project, he hired a palliative care doctor. Together they developed a curriculum to train primary care doctors on how to recognize that someone might be coming toward the end of life, and how to have those important conversations with them.
At the start of the program, 24% of patients were dying with hospice versus dying in the hospital. They continued to measure improvement post-education at six months, twelve months, eighteen months, and so on.
“To my surprise and appreciation, we significantly increased the percentage of patients dying with hospice, by a lot,” says Dr. Parker. “And for me, that’s all about better care. Now, it turns out that better care also saves a lot of money to the system. So in a capitated value-based care model, it’s a win-win, because it’s better care and it is saving a lot of money to the system.”
Thank you for reading
This article is just one in a series that explores how Arcadia’s ACO customers enrolled in the Medicare Cost Savings Program (MSSP) had another record year, generating $386 million in shared savings, and once again outperformed market benchmarks.
We’ve identified three areas of opportunity for ACOs that have helped our customers succeed in a changing marketplace:
- Transitional Care Management (TCM)
- End-of-Life Care
- Percentage of Members with Annual Wellness Visits (AWV’s)
To get access to all three articles in this series, subscribe to get notified when these are published. In the meantime, download the 7 Critical Capabilities of an ACO white paper, or book a consultation with an Arcadia expert.
