What are the 12 social determinants of health factors and why do they matter?
Social determinants of health (SDoH) are a hot topic in healthcare. In the past decade, they've emerged as one of the major focal points for organizations from private hospitals to NGOs. But what are they? Why are they important to measure? And how can they play a role in more efficient care with better patient outcomes?
Here, we'll walk you through the basic premise of SDoH measures, learning straight from Arcadia Senior Data Analyst Arjun Gosain about rapid developments in the field and how this concept might shape medicine in the future. Read on for a breakdown of key concepts.
What are SDoH (social determinants of health)?
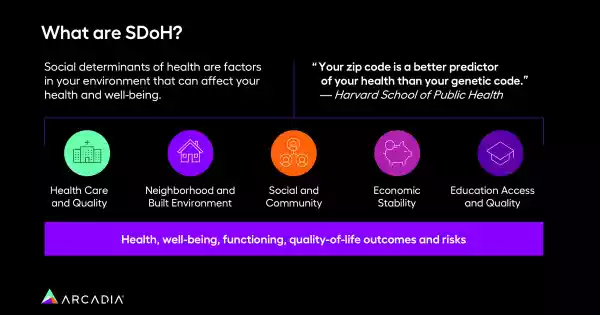
Health.gov defines social determinants of health as "the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks." Put more simply, they're the major factors outside of sheer biology that bear a major influence on someone's life. Someone with strict religious beliefs, for example, will view medicine through a different lens than an atheist; someone with darker skin may have experienced lesser care or discrimination in their attempts to be healthy.
The link between what happens outside a hospital's walls and within may seem tenuous, initially, but patients are people first. SDoH acknowledges that people are shaped by their experiences, from behaviors to genes.

What are the 12 SDoH factors we measure?
Centers for Medicare & Medicaid Services (CMS.gov) measures twelve SDoH factors, which map to Arcadia's data platform:
- Employment insecurity: Is the patient employed? Underemployed? Harassed on the job?
- Psychosocial circumstances: Is the patient going through court proceedings? Carrying an unwanted pregnancy? Exposed to war or regular trauma?
- Housing insecurity: Is the patient going home to a consistent place every day, or worried about where they'll land?
- Social adversity: Is the patient struggling to integrate into a new place or culture? Excluded, persecuted, or bullied?
- Transportation: Is the patient able to travel where they need to? Is public transit in their area lacking?
- Food insecurity: Where are the patient's meals coming from, and can they eat regularly?
- Education and illiteracy: If the patient can't read, or wasn't formally educated to a certain level, can they navigate hospital paperwork? Doctor's instructions for a chronic condition?
- Occupational risk: Does the patient work in a role where they're regularly exposed to toxins, like pesticides? Do they incur physical harm on the job site?
- Economic insecurity: Consider the effects of chronic poverty — is a copay manageable? What about a hospital bill? Rent?
- Lack of support: In situations ranging from divorce to the death of a loved one, support is a critical tool for a patient's individual health
- Upbringing issues: Has the patient carried trauma from an abusive childhood?
- Language: Can the patient understand written instructions? Can they communicate what ails them?
Even within the U.S., there's no standard for these measures — where CMS and Arcadia cite these twelve categories, other organizations choose different labels that might fit the populations they serve more specifically. Outside the U.S., the variance is even wider.
Why do SDoH measures matter in healthcare?
"A lot of papers out there tell you that the traditional model of healthcare delivery — which involves hospitalizations, encounters, healthcare, delivery, pharmaceuticals — they affect a person's health outcomes only up to 10 or 20%. So a majority of a person's health outcomes are really driven by the socioeconomic factors that we're talking about, which are termed as social determinants of health," Gosain explains.
In value-based care particularly, the urgency of gathering this information is obvious. When an organization is tasked with preventing negative outcomes, tackling the 80% of health driven by environment is a path to better performance.

The challenges posed by SDoH data (and how to overcome them)
SDoH presents a two-part challenge for healthcare organizations: gathering the data, then acting on it.
Gosain's seen improvements in recent years, but historically, there isn't a lot of coding done for patients adversely affected by SDoH. When a patient visits their primary care provider, is that doctor or nurse practitioner going to outright ask them whether they're unhoused? Or if they experienced abuse during childhood?
"SDOH, in general, is a topic where patients don't really go outright and disclose if there's something," Gosain explains. "You wouldn't be proud to disclose to people, 'I don't have a house' or 'I have food insecurity.' So it's very difficult to get those that kind of information, number one, documented. And if it's not documented, it's very difficult to collect that kind of data in the healthcare or tech setting, to really start reporting on that information."
Beyond data scarcity, the second issue is taking existing data, then measuring and making it actionable. Without a well-defined pool of patients, organizations can't draw meaningful conclusions, even if they are able to intervene. How do you measure the efficacy of a program when you can't differentiate between the people who need help and the larger population?

Zero in on a few key SDoH measures that matter
The answer to this overwhelming conundrum? Gosain says it's imperative to focus and narrow scope, but it also might be intuitive — go for the largest, most obvious impacted groups in your population first.
"If you have a higher percentage of homeless populations, or high potential food insecurity, we would really want to look at those populations first," he says. "That's what we call the 'low-hanging fruit,' and that's where you can design programs to really address those populations, which can impact as many people as possible in one go."
It sounds straightforward enough, but there's one catch — programming and initiatives need to be measurable. If an ACO decides to offer free ride shares to and from a provider's office, for example, they could establish benchmarks between those who participate in the program and those who don't, assessing any reduction in missed appointments or routine care.
Umpqua Health exemplified this approach when they offered air purifiers during Oregon's difficult wildfire season, preventing respiratory distress in their SDoH-impacted community.

Broaden SDoH data sources to uncover golden insights
Another key to success is pulling from a broad pool of data. With the historical scarcity of SDoH coding and records, it's critical that organizations and policymakers look wherever useful information can be found, whether it's claims or clinical notes. A data analytics platform like Arcadia might be a helpful tool in this effort.
"We have a lot of technology and advancements right now that enable us to look at surveys and assessments coming out of like the point of care directly, assessment right from the EHR systems of hospitals, and ingest those questions and answers," Gosain says. "Arcadia can map those question answers to particular NGS connects, which really makes a huge difference in identifying more populations who previously we couldn't because of ICD code mapping not being up to the mark."
The path to progress, powered by data
Adaptable technology and the emergent field of SDoH make a dynamic pair. In the ongoing fight against health inequity, SDoH factors are a helpful way to organize specific socioeconomic hurdles. Organized, contextualized information is the first step in mapping out an action plan.
Tune into our upcoming SDoH webinar to dive deeper into this intricate issue and learn how you can equip yourself with insight for the future of healthcare.
