Why data analytics are an ACO’s most strategic tool
Branching out from fee-for-service to risk-bearing contracts takes gumption
There are plenty of barriers that prevent accountable care organizations and IDNs from taking the leap.
The most formidable? Anxiety around downside risk-based payment models, and the challenge of balancing fiscal performance with exceptional quality in the care itself. It’s an impressive balance, and ACOs are at the vanguard of healthcare. With a rock-solid data platform as a foundation, liability transforms into opportunity.
To stay on top, you’ve got to constantly refine workflows, processes, and performance indicators. It’s not enough just to meet expectations — you can beat them. Analytics are the ticket to remaining on the cutting edge without teetering too far into the unknown. Below, we walk you through their critical role in an ACO’s success using a case study from an Arcadia partner. Then, we’ll show how we can put our data and team of experts to work for you.

Analytics lead to sustainable performance in value-based care
The first step in ensuring your ACO’s success is identifying ways to improve performance and push insights into clinical workflows. In short: identifying opportunities in the data, then actioning them in the real world where they can make a difference.
Then, once an initiative is in progress, you need to monitor performance to ensure you’re getting the desired return on investment. With that information to guide your strategy and negotiations, you’ll be able to handle more risk-based contracts and more contract complexity. But you’ll also need the right foundation of people, process, and technology to bolster your efforts.
That’s where Arcadia’s advanced analytics come in. We’re here to help you untangle the complex risk and population scenarios you face. After you’ve plucked the low-hanging fruit in value- based care (VBC) — like hospital readmissions and emergency department visits — analytics can help you succeed in increasingly complex risk-based payment models.
The data-driven difference for ACOs
Success depends on access to the right data, and making that data work for you. At a minimum, you need claims data combined with clinical information from electronic medical records (EMR), then supplemented by other sources available in or outside of your network.
When you drill down, metrics and data-driven insights can power better ACO performance by:
- Informing when and how to take on upside and downside risk and supporting more effective negotiations for VBC contracts
- Identifying the best opportunities for population health initiatives to make the most of investments
- Determining the impact your programs and infrastructure investments have on clinical and financial outcomes
- Providing reports that support well-aligned performance incentives as you build an organization of VBC believers
Five checkpoints on the road to optimal value-based care
This guide draws on the partnership between Arcadia Analytics and one of our ACO partners to give you a path to success. It raises five key criteria to measure the health of your ACO’s existing analytics, and to see opportunities where they could empower results:
- Assess whether your organization has the necessary analytical capabilities to support your VBC business
- Prepare to address data quality issues with external partners
- Plan an approach to acquire and implement analytics to drive specific high-value outcomes
- Use analytics to evaluate the performance of population health and VBC investments
- Identify high-value opportunities to leverage analytics to drive performance on a VBC contract
Baseline analytical capabilities
Your baseline analytical capabilities should support value-based care (VBC) growth strategy alongside fundamental fee-for-service (FFS) business.
What are these key capabilities, specifically? A foundational dataset, data-driven workflows, and enhanced analytics.
Robust dataset and analytics help identify opportunities that translate into workflows. You want to shape provider behavior and then determine if modifications produce hoped-for results.
The foundational dataset starts with claims data, yielding insights into out-of-network utilization that aren’t available in your own clinical systems. For a holistic picture, you need to integrate these with rich clinical data from multiple electronic medical record providers.
Beyond that foundation, other sources connect to an extended network of data that proves valuable for patient care. With this comes an essential consideration: what additional data your business needs, beyond what you have internally, and how you’ll access it. You’ll make constant tradeoffs between getting the best data and using what’s easily available.
Strong relationships with external partners are critical to the success of this auxiliary data.
Foundational dataset
- Eligibility and claims from health plan
- EHR data
- Notices of admission and ADTs
Data driven workflow
- Attribution management
- Coding compliance
- Quality performance
- Patient management
- Insights at the point of care
Enhanced analytics
- Access normalized dataset directly
- Calculate risk and impactability scores, quality measure compliance, and KPIs
- Generate scorecards to track performance

Common data quality issues that impact ACO and IDN performance
To build trust in analytics, consistency and accuracy are critical. To reach optimal success and efficiency, you need buy-in from everyone engaging with the data, from providers to analysts. Engaging and aligning providers on key goals goes hand-in-hand with setting clear imperatives around focal areas. Are you hoping to reduce visits to emergency departments? Screen a certain percentage of a demographic for pre-diabetes? Whether it’s pointed or sweeping, the flow of data from point of contact to a larger dataset needs to be seamless, and its quality unimpeachable.
This is the lodestar that guides our practices and workflows. High-quality data are fit for use — but that depends on correctness, completeness, integrity, validity, and relevance. Common issues include the following:
- Masking of sensitive diagnoses and procedures
- Omission of critical data fields
- Format changes when new elements are added or processes change
- Missing in-network and out-of-network indicators
- Time period variation in historic claims data
When providers understand the importance of data and how it translates to better patient care, their engagement leads to an enthusiastic, cooperative team. This means the data they receive should be high-quality, and the way they receive it should be transparent — you or a data partner (like Arcadia) must vet it before it ever reaches a care team’s hands, and once it gets there, it should speak to the specific benchmarks and goals your ACO has set. Below are a few steps to streamline that process.
- Verify on-time and complete delivery
- Monitor your data sources and ensure inbound data telemetry is run immediately
- Audit data quality to ensure it matches expectations set in your contract
- Negotiate the way you report and escalate discrepancies
- Resolve errors proactively to build trust
How analytics wrote this multi-state ACO’s success story
An ACO with locations across several states prioritized use cases where data should drive workflows. For example, active management of patient attribution is critical for success in accountable care. That information includes who your patients are, where they are, how sick they are, and what services they need to achieve optimal outcomes.
Enhanced analytics provided actionable insights at the point of care.
Direct access to normalized datasets let the analytics teams calculate performance on all critical components of VBC success. The analytics team generated scorecards that providers and care teams use to see how workflows improve health outcomes. As care teams grow in their ability to use the data to inform clinical workflows, enhanced and predictive analytics must also become more sophisticated for continued success.
As this network progressed deeper into their risk journey, adding data related to disease burden capture and coding gaps became critical. In this age of virtual care, telehealth, and remote physiologic monitoring, data are also essential for coordinated and comprehensive patient care. Finally, socio-demographic data help providers understand the social needs of patients, which are important influencers of health outcomes.
ACO by the numbers
We innovate with analytics to drive provider incentives, track ROI, and inform program investment:
- 340+ locations in New Jersey, New York, and Oregon, Connecticut, and Pennsylvania
- 275,000 attributed patients
- 12,000 employees
- 2,500+ providers
- 30+ value-based contracts
- 5-year engagement with Arcadia to deliver near real-time reporting and analytics for administrators along with actionable insights at the point of care
An analytics insight to scaffold healthcare innovation
This organization derives value from data in three key ways:
- Workflows — data informs day-to-day clinical workflows, stratifying patients and maximizing the value of each interaction
- Provider incentives — data gives providers real-time visibility into their performance and opportunities to improve care in the short term. Data also informs incentive programs for physicians as well as care team members
- ROI analysis — analytics enable assessment of population health program impacts and informs strategic decisions, including growth and program development and clinical workflows
Value creation as an ACO requires careful thinking to balance drivers in people, processes, and technology. In the debate over buy vs. build, it’s easy to overlook the numerous pitfalls involved in creating a data team from scratch. There are risks on both sides, but Arcadia mitigates these through best-in-class software and a full partnership — every time we approach a problem, we bring years of expertise and the discoveries made on behalf of our successful customers. In our ACO partner’s case, that meant closing 5.13% more risk for each patient that went through a particular chart prep workflow.
- Determine the level of support and partnership you need to accelerate your path to value
- Evaluate your internal analytics capabilities in terms of expertise and speed
- Invest in external partnerships to bring in best practices and advanced data science
and analytics - Manage internal and external resources effectively to ensure analyst, clinical, and operational teams collaborate effectively
The ACO chose to buy a custom technology solution for their use cases and priorities. The group focused on creating a partner in Arcadia who would grow and learn with them to use data for their three priority areas and drive the value for their ACO and other VBC contracts.

Use your analytics foundation to identify opportunities
You create value as an ACO by thinking about how you can balance value drivers: quality and patient experience, cost, and disease burden capture.

Improving patient outcomes creates success for ACOs in VBC contracts because cost savings often follow. For example, this example organization assessed skilled nursing facilities (SNFs) to determine if they were able to get patients home safely and reduce length of stay and readmission rates, ultimately producing cost savings. Using Arcadia’s data analysis to guide daily workflows and discharge planning efforts, they determined that their efforts did reduce overall SNF days per thousand, the major cost driver in a Medicare ACO.
Arcadia and our ACO partner also analyzed annual wellness visit (AWV) impacts. The analysis looked specifically at whether AWVs were improving quality outcomes, capturing disease burden, and encouraging loyalty. An earlier AWV strategy boosted visits to over 75% of the eligible population. The healthcare system wanted to determine if AWVs produced a real impact on the population.
The results demonstrated improvements in patients’ lives, and increased resources for the ACO. Their initiative unlocked a 9% increase in revenue, with potential to reach 15% through program success.
We also worked with our ACO partner to see if they could leverage medical specialty pharmacy services to increase patient retention and capture additional FFS revenues. The analytics showed that the same infusion done in a hospital-based ambulatory facility costs significantly more than in an ambulatory infusion center — and this healthcare organization has its own infusion center.
Moving patients to the ACO’s facility greatly reduces cost of care. Continuity of care and patient experience improved, increasing retention of infusion services. In reducing costs, revenues increased. Additionally, data on dosing showed that this healthcare system could optimize both dosing and medications for better outcomes.
Impact of annual wellness visits on patients
- 8% higher quality gap closure
- +1.7 additional office visits over 6-month period post AWV
- 9% higher year-over-year retention in the attributed population
- 0.11 higher risk factor for members with AWV
The AWV population saw significantly better closure of quality gaps and enhanced outcomes, so long as they remained attributed to the ACO — which, in turn, increased adherence to the group.

Use your analytics foundation to evaluate performance
A key to success in VBC is managing and motivating a mixed group of employed and independent providers to engage in programs and drive outcomes. Providing appropriate incentives for performance certainly helps.
This ACO’s goal was to reward physicians who proactively manage their panels and make the greatest positive impact on VBC contracts and patient outcomes. Arcadia developed sophisticated metrics to appropriately identify and incentivize physicians based on quality scores, disease burden accuracy, and utilization metrics.
How did they approach this opportunity? They assessed each primary care provider’s panel and determined their risk-adjusted admissions per 1,000, and impact on the group’s overall quality performance. Based on those two factors, the ACO was able to give primary care providers appropriate incentives along with actionable data to continually improve.
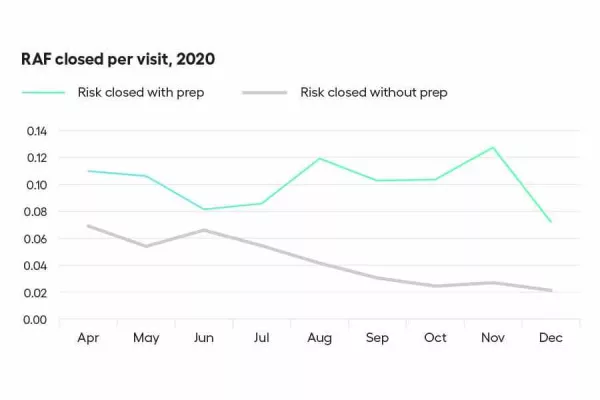
Chart prep in clinical workflows offered another potential high-value opportunity. The ACO wanted to identify meaningful gaps in disease burden capture and present them to physicians before patient encounters. In addition, the group wanted to evaluate the impact of chart prep by coders.
Analytics empowered our client to identify and inject insights into clinical workflows. Risk coders use claims and EHR data to suspect chronic conditions and stratify patients by opportunity. A registry lists patients with upcoming appointments. Before the appointment, coders prep charts and communicate actionable gaps to physicians within clinical workflows. Analytics allow measurement of the impact of chart prep in clinical workflows. The result was a 30% increase in risk gap closure.

Build analytics performance to meaningfully and directly impact success in VBC and FFS contracts
This ACO’s approach demonstrates the value of bearing additional risk in incremental progressive steps. You can utilize a similar tactic.
Analytics informs when and how to take on upside and downside risk and provides data critical for negotiations to develop win-win arrangements. Identifying the best opportunities to create new population health initiatives helps deliver the greatest return on investments. A sustainable ecosystem — where finances and delivery of care are both at optimal performance — is built on incremental changes. With analytics in place, one success begets another, enabling further investments in VBC and determination of program impacts on clinical and financial outcomes. Finally, analytics supports well-aligned performance incentive programs and growth of an organization of true VBC believers. Start the conversation to learn more.
