Introducing the Ambulatory Specialty Model
Early detection and management of chronic disease can improve health outcomes for patients while also decreasing the overall cost of their care. Unfortunately, care delivery is increasingly fragmented between specialists and primary care providers, creating care gaps that can work against the benefits of early detection and management.
In July 2025, The Centers for Medicare & Medicaid Services (CMS) proposed the Ambulatory Specialty Model (ASM) as part of the 2026 Medicare Physician Fee Schedule rulemaking. This five-year model, launching January 1, 2027, will be mandatory for specialists in 25% of core-based statistical areas (CBSAs) treating heart failure or low back pain in outpatient settings. According to CMS, these two chronic diseases cost a combined $16-21 billion annually in the Medicare population and often have instances of low-value care.
Key features of ASM
Mandatory Geographic-Based Participation:
Certain specialists in 25% of CBSAs (regions to be selected at a later date) who treat 20 or more low back pain or heart failure episodes annually will be required to participate.
Performance is assessed in four categories:
Quality, cost, improvement activities, and promoting interoperability—modeled after MIPS Value Pathways (MVP) but with condition-specific measures. A single score of 0-100 is created from the four categories with quality and cost representing a vast majority of the score (up to 100 points).
Payment years are two years after the performance year.
For example, performance year 2027 will impact payments to specialists in 2029. Providers will be compared to other providers within their CBSA utilizing the score calculated above and fees paid to these providers will be adjusted from –9% to 9% for the first performance year, increasing to –12% and 12% by the final performance year. These adjustments ensure that the positive adjustments for high performers do not total more than the negative adjustments for low performers.
Requirements demand practice transformation
The ASM establishes rigorous requirements for participating specialists beginning January 1, 2027. Heart failure specialists must demonstrate blood pressure control capabilities and coordinate care seamlessly with primary care providers, while low back pain specialists face mandates to improve patient functional status and reduce unnecessary interventions, such as MRIs. Both specialties must establish formal collaborative care arrangements that define clear roles for data sharing, co-management protocols, and joint responsibility for screening for health-related social needs.
The model leverages the MVP framework across four critical performance categories. Quality measures focus on specialty-specific outcomes that specialists can directly influence, moving beyond generic metrics to condition-specific improvements. Cost performance emphasizes reducing avoidable care through episode-based measurement, with specialists accountable for the full continuum of care during defined episodes. Improvement activities require enhanced care coordination, mandatory social needs screening, and patient safety initiatives. The promoting interoperability category mandates Certified Electronic Health Record Technology (CEHRT) adoption with robust data sharing capabilities.
Data is critical for success
ASM scores providers primarily on cost- and episode-specific quality measures. Once a score is calculated for a provider, every provider score within a CBSA is compared to identify which providers will have positive, negative, or neutral adjustments to their reimbursement. This means that providers need to understand not only how they are performing along each measure at an individual level, but also how that compares to every other participating provider in their CBSA.
Turning to a specific example, low back pain episodes in Dallas, Texas, you can see in the chart below every provider that would be required to participate in ASM in the Dallas CBSA and their average low back pain episode costs for 2024. Highlighted in orange is a specific provider whose average episode cost falls well over the median cost for Dallas (represented by the dashed line). Approximately half of the ASM score is comprised of cost, meaning this provider is at significant risk of seeing up to 9% decrease in reimbursement for low back pain services under the model, according to the 2026 Medicare Physician Fee Schedule.
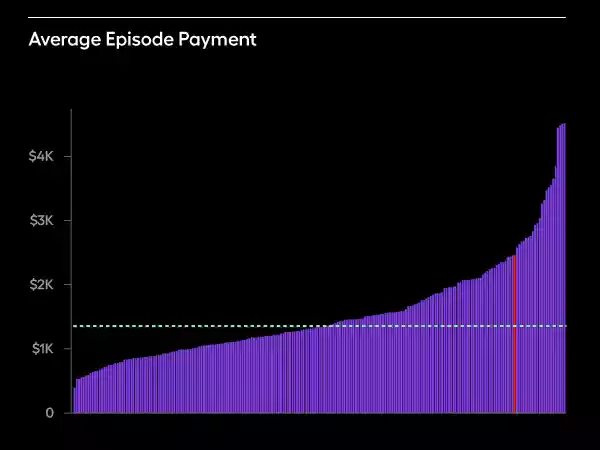
Source: CareJourney by Arcadia Provider Intelligence Data (2024)
The other half of the score is comprised of a series of quality measures. For low back pain, these measures are: (1) utilization of MRI; (2) use of high-risk medications; (3) depression screening and follow-up plan; (4) BMI screening and follow-up plan; and, (5) improved functional status. Other measures are under consideration, but CMS has so far only proposed these five. The chart below shows the frequency with which providers in Dallas utilize MRIs in low back pain episodes with the same provider highlighted in orange. The provider that was well over the median cost per episode utilizes MRIs less frequently than their peers, meaning they would score higher on this quality measure.
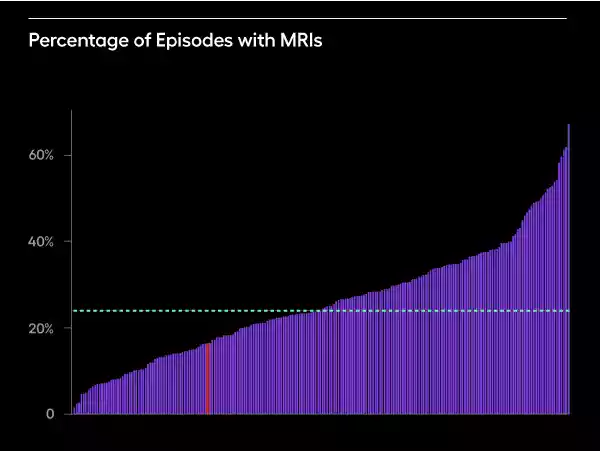
Source: CareJourney by Arcadia Provider Intelligence Data (2024)
How can our highlighted provider change their practice to be more successful under the model? They need to move their average episode cost closer to the median, which requires understanding why their average episode costs are high. Arcadia’s provider performance data enables providers to understand the cost breakdown of their episodes. In this instance, the highlighted provider performs more spinal fusion surgeries on low back pain patients than their peers—a high-cost intervention that pushes their episode costs higher than their peers. The provider performs spinal fusion surgery on approximately 7% of their low back pain patients compared to a median of approximately 2%.
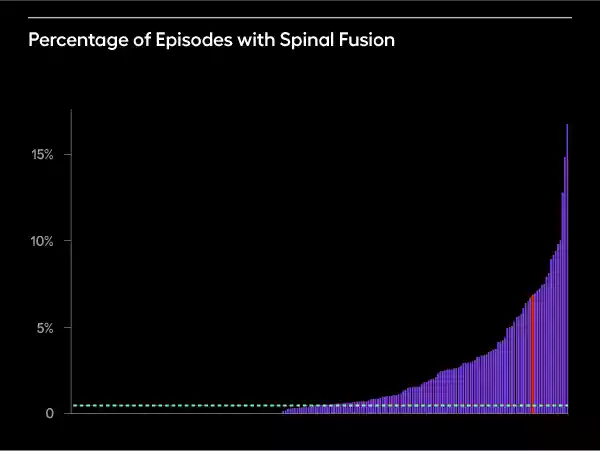
Source: CareJourney by Arcadia Provider Intelligence Data (2024)
Technology infrastructure improves success
To succeed in CMS’ ASM model, provider organizations will require robust data infrastructure and advanced analytics tools that align with the model’s requirements. Three technology-enabled capabilities are especially critical:
1. Performance Intelligence for Transparency and Benchmarking
Success in ASM hinges on transparency and the ability to benchmark performance across large populations and peer groups. Look for solutions that offer:
- Access to nationwide and market-level analytics that encompass hundreds of millions of beneficiaries and millions of providers.
- Risk-adjusted scoring methodologies that enable reliable comparisons across provider performance.
- Episode-based cost measurement frameworks that align directly with conditions prioritized under ASM, such as heart failure and low back pain.
These capabilities allow organizations to understand relative performance, surface variation, and drive targeted improvements—all foundational to ASM’s transparency and accountability goals.
2. Point-of-Care Insights to Drive Quality Measurement
ASM places a strong emphasis on chronic disease management and quality measurement. Tools that surface longitudinal patient data within clinical workflows—without disrupting provider efficiency—are essential. Capabilities that participating organizations need include:
- EHR-integrated decision support for timely access to comprehensive patient histories.
- Intelligent risk stratification to proactively manage high-risk populations.
- Automated quality gap closure workflows that align with ASM’s reporting and incentive structure.
These insights empower providers to make informed decisions in real-time, which is critical for improving outcomes under ASM’s quality-focused framework.
3. Technology-Enabled Care Coordination for Targeted Conditions
Effective care coordination is required under ASM, especially for high-cost, high-need patients with heart failure or low back pain. Look for technology that can:
- Predictively identify high-risk individuals using condition-specific models.
- Automate workflow routing to streamline care team operations and reduce administrative burden.
- Embed evidence-based guidelines into care planning, supporting consistent, high-quality interventions.
Arcadia's comprehensive healthcare data platform aggregates clinical, claims, social determinants, and pharmacy data in real-time. Our platform's proven value-based care success—including 41.5% ED visit reductions for COPD patients and enabling care teams to serve 3x more patients—demonstrates the capabilities needed to drive ASM-required outcomes.
