How to surface data at the point of care to serve complex populations
How does a healthcare organization serve the populations that traditionally are the most overlooked by the healthcare system?
Belong Health, which serves complex populations such as special needs or dual-eligible for Medicare and Medicaid populations that have been traditionally underserved by the healthcare system, centers its model around patient care and care management. It’s driving better clinical outcomes through enhanced customer service.
In Arcadia’s Byte-Sized Insights, Belong Health’s Vice President of Operations- Stars and Risk Adjustment, Jeff Cox, and Vice President, Digital Product and Data, Mac Davis, describe how execution of risk adjustment and quality is central to driving growth.
Risk adjustment drives growth
Davis says people often see risk and quality in a silo and don’t appreciate how embedded risk and quality performance is in their performance in a variety of functions. Instead, it should be thought of as a driving force for performance across all key stakeholders within the health plan.
“If you’re not executing on compliant risk adjustment to the same degree as other competitors in the market, you’re losing out on potential revenue that is going to drive how you fund the benefits in your product, it’s going to change how you present yourself, and provide for some of those members,” Davis explained.
Growth tends to drive from the ability to fund functions, so without risk adjustment, growth is not possible.
As new CMS rules take effect documentation must be error-free
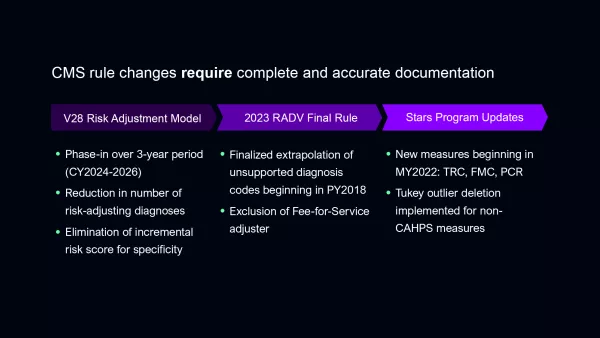
As the Centers for Medicare and Medicaid (CMS) implement the new V28 Risk Adjustment Model for Medicare, the RADV Final Rule, and the Star Ratings Program updates, the need has never been clearer for documentation to be 100% accurate.
V28 will result in a significant reduction in the number of ICD-10 codes that tie to HCCs and the elimination of the incremental risk score for increased specificity for certain diseases such as diabetes. In addition, the RADV Final Rule’s exclusion of fee-for-service adjuster adds pressure to plans. And finally, Star Ratings will have three new utilization-based measures of care and several other programmatic changes that change the way the Stars Ratings are calculated.
“Make sure documentation is 100% accurate, because that should be the expectation and CMS is decreasing the regulatory acceptable margin of error,” Cox said.
Every action around Star Ratings and quality must be reflected in the medical record so that it can be validated when the organization gets audited.
Promoting annual wellness visits
Belong promotes annual wellness visits which they believe encourages relationships between members and providers. It also allows the organization to get a comprehensive, complete documentation of code submissions and quality gaps as well as complete health risk assessments.
“One way we’ve helped to promote higher quality documentation during those encounters is through leveraging Arcadia Assess which helps to surface suspected conditions as well as open quality gaps for that specific patient and provides medical record documentation for the provider to address,” Cox said.
Davis says Belong has increased its annual wellness rates for its members by 122% from the previous year, doubled its membership year-over-year, and has driven adverse utilization events down by enforcing comprehensive and deep relationships with primary care providers.
“It goes back to making the most of every encounter we have with a patient whether that is first call resolution with our care team or comprehensive and member relevant annual wellness visits,” Davis said.
To be successful, it is important to recognize what specific barriers the practices you’re working with face.
“Understanding what those challenges are and deploying out scalable, tailored, and tactical solutions for each practice is critical,” Cox explained.
Driving better outcomes
Diverse interventions can address many important goals across large complex networks. Using data to build a strong operational foundation is critical. Watch more Byte-Sized Insights or request a demo to see how we can put your data to work, together.
