Healthcare dashboards: 8 impactful models + metrics to track
Making informed, urgent decisions is an absolute must for healthcare professionals. However, wading through overwhelming pools of data can drastically decrease the accuracy and efficiency of these health-related choices.
This is where healthcare dashboards provide immediate clarity and context. Healthcare dashboards are powerful analytics tools that accelerate performance by empowering healthcare professionals to incorporate relevant, updated data insights into their decision-making processes. In this guide, we'll explore what this looks like for healthcare organizations, including:
- Benefits of healthcare dashboards
- Healthcare dashboard metrics to monitor
- 8 healthcare dashboard examples
Once you realize the functionalities and benefits of analytics dashboards, the next step is to experience their full power for yourself.
Benefits of healthcare dashboards
In the dynamic and demanding world of healthcare, all organizations can benefit from healthcare dashboards. These analytics tools make data more accessible and enhance enterprise-wide performance, allowing users to:
- Simplify and organize data: With the ability to zoom in and out of various healthcare aspects, organizations can see a variety of data sets in fine-grain detail. By recording all critical data within a centralized location, healthcare dashboards make scattered, executive ad hoc reports a past relic.
- Forecast trends: A holistic view of data from various sources equips users to monitor ongoing health situations and forecast future trends. Using machine learning, these tools leverage predictive analytics to generate accurate predictions using past and current data.
- Improve care: With healthcare dashboards, healthcare professionals can quickly transform valuable insights into improved enterprise-wide performance. The result? Enhanced patient treatment and profitability across all major stakeholders.
Modern healthcare dashboards — like Arcadia Vista — make data more accessible for analysts and leaders by providing a growing library of healthcare intelligence dashboards built on top of a data platform optimized for value-based care.
Arcadia Vista simplifies and secures data insight distribution while managing contracts and providing return on investment (ROI) projections across specific lines of business. Before you know it, Arcadia Vista will revolutionize your organization’s operational efficiency. To gain a deeper understanding of healthcare nuances, continue reading to discover how to leverage our dashboard capabilities.
Healthcare dashboard metrics to monitor
Different dashboards extract different healthcare dashboard metrics. Below is a list of the most important metrics to monitor.
Patient satisfaction score
The patient satisfaction score reflects how patients perceive the quality of care and services healthcare facilities provide. Health professionals determine this score by assessing patients’ satisfaction with factors such as:
- Treatment outcomes
- Wait times
- Facility amenities
Data from patient surveys and other feedback tools enable providers to assess the elements impacting patient satisfaction. When visualized through a healthcare dashboard, this data can even reveal long-term trends relating to patient-centric process improvements or gaps in care.
A high patient satisfaction score indicates a patient’s positive perception of a provider, which can ultimately lead to improved provider loyalty and reputation. Low scores, on the other hand, reveal opportunities for improvement.
Transitional care management (TCM) data
Transitional care management (TCM) addresses the hand-off period between the inpatient and community setting. Relevant statistics show outcomes related to members who had a TCM visit billed by a physician following an inpatient discharge in which the patient was discharged to home, with or without home health.
Average length of stay (ALOS)
The average length of stay (ALOS) measures the number of days, on average, a patient spends admitted to a healthcare facility. To find the average, divide the total days patients spend in the facility by the number of discharges within a specific time period.
This metric enables providers to balance efficiency with quality of care. For instance, an extended stay increases the risk of developing other complications, such as acquiring a new infection from a hospital. However, releasing a patient too early could result in costly readmissions.
Contract summary data
This data tracks medical costs and utilization trends to inform payer-provider decisions. Contract summary metrics include:
- Medical and pharmacy costs and utilization
- The impact of high-cost claimants
- Enrollment changes over time
When tracking contract summary metrics, timing is key. Payers should be able to view cost and utilization metrics in rolling 12-month or calendar year periods and evaluate trends from the previous period. This view allows payers to see high-cost claimants' impact on PMPM and visualize member enrollment trends over time.
Readmission rate
Readmission rate refers to the percentage of patients who are readmitted to the facility within a specific time frame. Healthcare dashboards allow providers to monitor readmission trends, contributing factors, and the impact of interventions on reducing readmissions.
Cost per treatment
The average cost associated with a specific procedure or treatment may reveal opportunities for cost reduction without sacrificing the quality of care. To measure cost per treatment, health professionals must analyze all costs tied to the treatment, including:
- Direct costs that are attributable to the specific procedure, such as staff time and medical supplies
- Indirect costs which are necessary for the facility’s operation and aren’t directly tied to a particular treatment
Healthcare dashboards consolidate data across procedures, ensuring stakeholders have a holistic view of all relevant information. This way, health professionals can compare costs across procedures, identify outliers, and monitor financial efficiency.
Skilled nursing facilities (SNFs) performance
Assess individual provider and facility performance by analyzing high-level inpatient trends and KPIs like:
- Average SNF length of stay
- Referral sources
- % of SNF patients discharged home vs. readmitted
These metrics help health professionals identify facilities and providers in comparison to plan product and DRG-adjusted averages.
8 healthcare dashboard examples
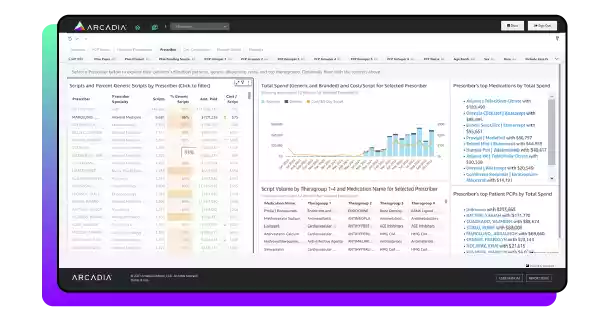
1. Quality Performance
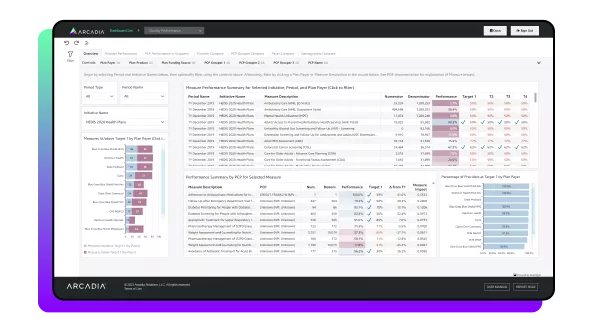
Quality performance KPIs
- Performance vs Target
- PCP’s Measure Impact
- PCP’s Overall Quality Rank (sum of measure impacts)
To efficiently care for patients while maintaining peak functionality, healthcare professionals must consistently evaluate their operational performance. Doing so ensures that their revenue streams remain profitable across all sectors. Healthcare quality performance dashboards give an adjustable bird’s eye view of performance management.
Arcadia’s quality performance dashboard measures the comparison between healthcare payers, primary care providers (PCPs), and additional healthcare providers all within a single initiative. Users can select an initiative and time period on the overview tab, and then easily view performance by PCP accompanied by a Measure Impact score. The Measure Impact score indicates to what degree an individual PCP positively or negatively “moved the needle,” impacting a network’s performance.
Three additional tabs allow users to compare entities (PCP, Payers, or PCP Groupers) in relative quality measures. Finally, a demographics tab highlights any variation in performance across lines of race, ethnicity, sex, language, and age.
Quality performance dashboards offer an adjustable solution to performance and operational decision-making by providing a clear window into your organization’s efficiency. From these metrics, you can formulate actionable fiscal and administrative recommendations for an increased ROI.
2. Transitional Care Management (TCM)
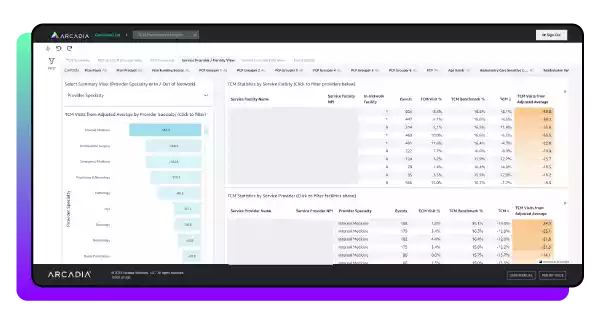
Transitional Care Management KPIs
- TCM Visit %
- TCM Benchmark Visit %
- TCM Visits from Adjusted Average
Following an inpatient stay, there’s a phase known as transitional care management (TCM), which involves dedicating resources and time to managing a patient’s transition out of the hospital.
This phase usually occurs within a set 14-day management cycle following an inpatient medical or surgical discharge. In this phase, the discharged patient goes home with or without home health. TCM’s main objective is to ensure the patient is not readmitted to a hospital during this transitional period.
Effective data hygiene is necessary for every successful TCM program so that providers can measure changes after hospital discharges. That’s why a TCM dashboard is incredibly useful for providing insights following inpatient procedures. Reported metrics like visit rates, adjusted average benchmarks for PCPs, facilities, and providers, and PCP scorecards give context for TCM performance.
Users can also adjust views to read a TCM summary and then move into analyzing TCM across a PCP Grouper view and DRG (diagnosis-related groups) view for event details. Effective TCM tracking and analysis improves administrative workflows and offers insights for providers to identify and close gaps during this critical period.
3. Ambulatory Surgery Centers (ASC)
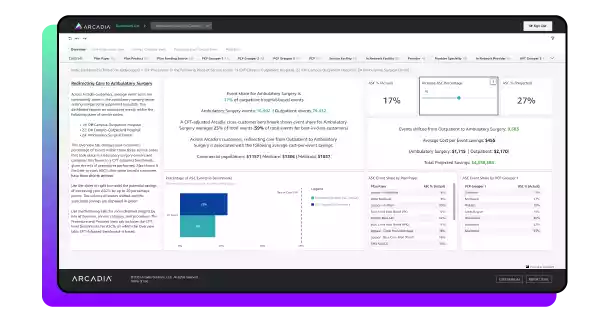
Vista Ambulatory Surgery Centers KPIs
- Percentage Events ASC
- Cost per Event
- Facility Type
Surgeries within ambulatory surgery centers (ASCs) do not need hospital admission. They are cost-effective and convenient in comparison to traditional outpatient hospital settings. However, without proper data tracking and analysis, many providers do not know exactly how much more cost-effective ASCs are.
Arcadia’s dashboard compares the exact cost per event in ASCs and outpatient settings. Correspondingly, it allows users to model the potential savings of shifting care from outpatient to ASCs by contract type. This means that users can make informed decisions based on cost and event trends available in four distinct views:
- Line of business view
- Service category view
- Procedure view
- Provider view
ACO Leaders and Business Analysts can then leverage cross-customer benchmarks to investigate the percentage of events performed in ASCs with the ASC percentage slider. Arcadia customers can know the true difference in cost with a robust ASC dashboard.
4. High-Cost Members
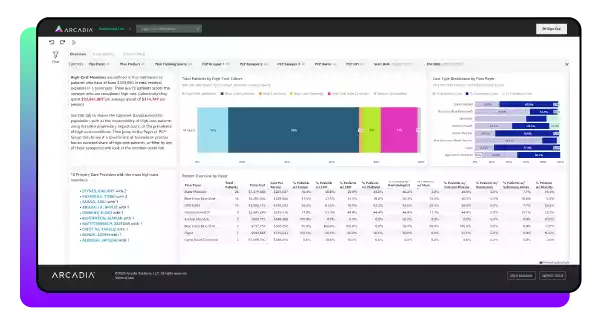
Vista High-Cost Members KPIs
- High-Cost Cohort (Admission, Condition, Drug, Maternity, Rare Condition, Unclassified)
- Cost Type (Inpatient, Outpatient, Pharmacy)
- Impact Score Category (Arcadia Arc Score)
- Condition by Impactability (Very Strong Potential, Strong Potential, Good Potential, Some Potential, Not Recommended)
- Total Members
- Total Cost
Factors like chronic conditions, expensive medications, and maternity cases identify some patients as high-cost members within a healthcare organization’s framework. Arcadia differentiates these members from others by focusing on those with over $200,000 in calendar year spend.
The Arcadia Vista High-Cost Member dashboard provides a member overview and then breaks members into high-cost cohorts and cost types by Plan Payer. Additionally, the Impactability tab shows conditions and PCP Groupers by impact score categories. Finally, the Patient Detail tab offers several filters for a more in-depth patient view.
These patient filters include:
- Impactability
- High-cost cohort
- Minimum total cost
- PCP visits
Arcadia’s Vista High-Cost Members dashboard categorizes patient data into several comparable tabs to give users an informed look into high-cost members. This dashboard has a variety of KPIs to best capture patient data.
5. Social Determinants of Health (SDoH)
Vista Social Determinants of Health (SDoH) KPIs
- SDoH PMPM
- Population PMPM
- SDoH Concepts
- Member Count
- SDoH Condition Prevalence
- Avg. IP Stays per Member
- Avg. ED Visits per Member
Social Determinants of Health data (SDoH) are some of the most crucial factors an organization can use to mitigate risk and improve patient outcomes while experiencing financial success. This data explains what’s happening in a patient’s life outside of healthcare waiting rooms so that PCPs can provide top-notch care without sacrificing time investigating outside factors.
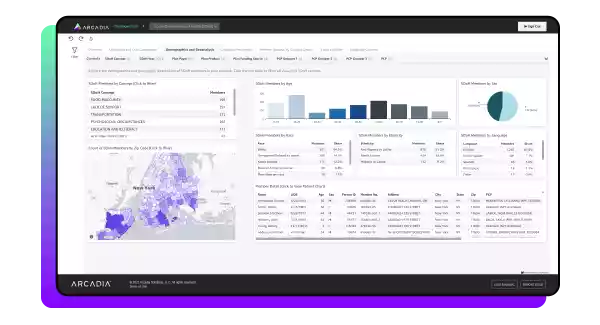
Arcadia Vista’s SDoH dashboard identifies SDoH challenges through analysis of claims and critical data in addition to care management and clinical assessments. All of these insights are then sifted into seven distinct tabs:
- Utilization
- Spending
- Demographics
- Geoanalysis
- Condition prevalence
- Language concerns
From there, users can switch between complementary Vista dashboard tabs such as the Member Analysis and Cohort Builder tabs to dissect the impact of these patterns and view member-level details.
When furthering health equity is the goal of SDoH data analysis, users need a robust software solution to help them gather new insights and uncover population health patterns. That’s why Arcadia Vista makes healthcare equity initiatives achievable.
6. Benchmarking
Benchmarking KPIs
- Cost of care
- Service utilization
- Risk score
- Performance quality
Healthcare organizations must benchmark their internal performance against external, market-based standards to truly excel in value-based care. This comparative analysis helps organizations identify performance blind spots, uncover opportunities for improvement, and adopt best practices to enhance care quality and operational efficiency. Healthcare benchmarking dashboards offer comprehensive insights across providers, practices, facilities, and entire networks.
Arcadia Vista empowers healthcare organizations to access these insights with integrated benchmarks powered by CareJourney’s market intelligence and Arcadia’s de-identified dataset of over 20 million lives across multiple payer types. These benchmarks allow organizations to:
- Analyze cost, quality, and utilization metrics against national, regional, and peer-level standards
- Identify high-performing providers and practices and emulate successful models across the network
- Detect underperforming areas and implement targeted practices to improve outcomes
7. Network Integrity
Network Integrity KPIs
- Provider efficiency scores
- Referral patterns
- Capacity utilization
- Attribution trends
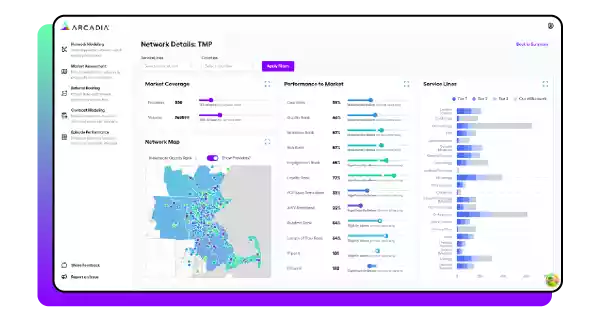
Network integrity reflects a health system’s ability to retain patients within its defined provider network. Understanding patient retention enables providers to enhance care coordination by refining their referral processes and more efficiently utilizing resources. To accomplish this, health professionals must analyze their market share in the network by tracking patients through the continuum of care.
Arcadia Vista’s network integrity dashboard offers comprehensive insights into patient retention and leakage patterns. The dashboard offers both high-level summaries and granular analysis, including spending patterns in and out of the network during critical periods, such as the 90 days following new specialist visits.
Healthcare organizations can use Arcadia’s Network Modeler to design, build, and evaluate networks at scale. Powered by data from over 745,000 providers nationwide, organizations can:
- Identify high-performing providers to expand into new geographies strategically
- Optimize existing networks to balance cost, quality, and access
- Gain visibility into population statistics to address disparities and promote health equity
8. Polypharmacy
Polypharmacy KPIs
- Medication count per member
- Pharmacy cost trends
- High-risk medication prescriptions
Polypharmacy is the use of multiple medications by a single patient. This poses significant risks if not properly managed, including harmful drug interactions, reduced medication adherence, and unnecessary healthcare costs.
Healthcare organizations must address these risks by identifying impacted patients, simplifying the care management team’s processes, and preventing unnecessary overmedication. Healthcare polypharmacy dashboards support this by highlighting harmful drug combinations and drug cascades and analyzing medication use across patients.
Arcadia Vista’s polypharmacy dashboard supports clinical pharmacists in identifying members with the most distinct medications in a 90-day window and members with potentially harmful or costly drug combinations. This not only helps reduce adverse drug events but also improves patient outcomes by enabling targeted interventions.
Arcadia Vista: Healthcare dashboard software to empower clinical and operational care teams
Ready to take your data analysis to the next level? Partner with Arcadia Analytics and unlock the power of Arcadia Vista dashboards. Our self-service dashboards are purpose-built for healthcare business intelligence by utilizing a built-in value-based care platform.
Analysts and leaders benefit from Arcadia’s growing library of healthcare dashboards, which enable them to identify healthcare trends and holistically view population health. With Arcadia Vista, you can make your organization’s decisions count while empowering data-driven innovation. Discover your data’s story, partner with Arcadia, and experience the data-backed difference.
