Risk adjustment software overview + 15 top vendors in 2025
Risk adjustment is a critical process that involves providers, payers, and healthcare administrators in the value-based care landscape. It plays an essential role in ensuring equitable healthcare delivery and reimbursement.
Given the complexity of risk adjustment, healthcare teams need modern software solutions to manage patient data efficiently and calculate risk scores at scale. In this guide, we’ll cover the key concepts and top vendors to keep in mind when researching risk adjustment software in the following sections:
- Risk adjustment software FAQs
- What to look for in risk adjustment software
- Leading risk adjustment software vendors
Whether you’re exploring the concept of risk adjustment or ready to choose a vendor, this guide will show you how technology is revolutionizing healthcare risk management, optimizing patient outcomes, and promoting financial sustainability.
Risk adjustment software FAQs
Risk adjustment analytics use a statistical method to predict the likelihood of a patient group’s use of healthcare services, plus the associated costs. The method equates a patient’s health status to a number called a risk score to predict healthcare costs.
First, providers submit diagnostic codes on claims data that define a patient’s risk score. Payers then rely on accurate risk adjustment analytics to build health insurance plans. This payer-provider collaboration is essential for maintaining cost and quality standards across individual patient groups. In turn, effective collaboration ensures patients receive appropriate compensation while supporting the equitable and efficient distribution of healthcare services.
Risk adjustment software is a specialized tool used to analyze patient data and perform risk score calculations.
In the past, traditional healthcare systems relied on paper-based workflows to finalize quality programs. This forced health plan quality and risk teams into a cycle of “chart-chasing” to capture evidence and verify risk and quality data, leading to decreased efficiency, underwhelming performance, and stifled communication.
Cloud-based and integrated risk adjustment software solves this problem by reinventing the paper-based workflow and reporting structure. The software enables providers to identify and document suspected diagnoses at the point of care. Furthermore, networks can use this information to increase transparency and close risk gaps. This leads to higher reimbursement and reinvestment into better value-based patient care.
When providers embrace risk adjustment software, their workflows become simpler and more efficient. Watch this video for a closer look:
As described in the video, the risk adjustment process involves three steps — suspect, engage, and assess:
- Suspect: EHR-integrated software enables care teams to surface suspected risk gaps in patient care. These are areas where a patient’s risks are not fully accounted for in their records. The software uses integration and analysis to flag these risks based on treatment history, diagnosis codes, and clinical data.
- Engage: The next step is to automate patient engagement with AI-powered care management tools, such as appointment reminders and follow-up instructions based on individual patient profiles and risk assessments.
- Assess: In the last phase, payers and providers use software to create workflows according to the identified risk gaps. This could include additional screenings, follow-up appointments, or interventions.
With the right software, care teams can provide improved patient experiences and unlock increased savings from proactive resource allocation. This results in a win-win-win outcome for patients, payers, and providers.
What to look for in risk adjustment software
To generate accurate cost predictions, providers must have access to a variety of data, such as inpatient, pharmacy, social determinants of health (SDoH), and other point-of-care insights. This is where EHR-integrated risk adjustment software comes into play. When narrowing your software search, here are a few essential features to prioritize:
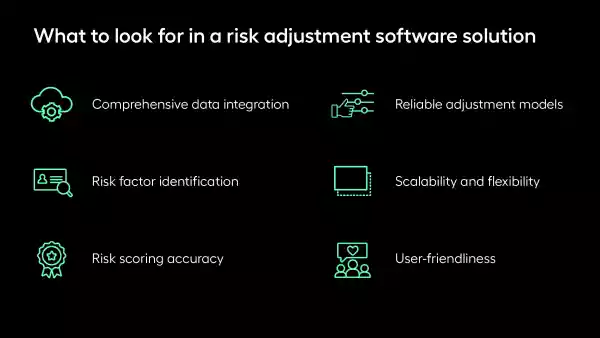
- Comprehensive data integration: The solution you choose should have high-powered integration capabilities so you can process data from multiple sources with confidence and pave the way for more accurate risk assessments.
- Risk factor identification: To plan informed and targeted interventions, your providers need to rely on a system that easily pinpoints high-risk patients. Without this capability, your team won’t be able to properly allocate resources and increase care efficiency.
- Risk scoring accuracy: This feature is a cornerstone of risk assessment since inaccurate scoring can lead to inaccurate payment for services and directly affect financial and operational sustainability and patient care quality.
- Reliable adjustment models: Look for a solution that offers a standardized approach for meaningful comparison across different patient groups, providers, and periods. That way, you can be confident in your benchmarking, performance assessment, and healthcare planning decisions.
- Scalability and flexibility: As your organization evolves, your software should adapt along with your needs. Find one that easily keeps up with changing patient population trends, regulatory expectations, and increased operational demand.
- User-friendliness: Healthcare providers need to be able to efficiently navigate your platform. A user-friendly interface is necessary for care teams to adopt the system into their existing workflows without extensive training.
Study vendor reputation and compare their services to your immediate and long-term needs. In addition to accessing the right features, it’s essential to find a vendor who has helped similar teams achieve the outcomes you’re looking for.
Best risk adjustment vendor: Arcadia
As a KLAS Featured IT Vendor, Arcadia simplifies risk coding and documentation to provide clear visibility across your entire network. Our comprehensive risk adjustment application library can help you unearth meaningful data points and drive healthier outcomes. Here is an overview of each featured application:
- Healthcare data models built by analysts, for analysts, to place quality, risk, financials, contracts, and clinical data into a simplified schema.
- Analytics dashboards to empower clinical and operational care teams to create customizable workflows and extract insights from massive volumes of data.
- Healthcare reporting for providers simplifies meaningful report creation and distribution to executives and other stakeholders.
- Point-of-care insights available within your existing EHR workflows that present actionable opportunities for providers to address risk gaps at the time of treatment.
- Provider-payer collaboration through cloud-based, configurable workflows to accommodate real-world variation between payers, health systems, and state requirements.
- Unified SDoH data that streamlines the population identification process to direct providers to groups in need of immediate care.
Additionally, our HCC Risk Suspecting App aggregates data from multiple sources (claims, EHR, APIs, SDoH) and then enriches it with a proprietary risk-suspecting engine. The app integrates payer and EHR data into a single data asset, enabling diagnosis suspecting from notes, labs, orders, and vitals. Get a closer look in the video below:

Advantasure
Advantasure provides comprehensive and balanced risk adjustment solutions to achieve complete and compliant risk score accuracy. Their specific services include:
- Bid process input
- Data-driven strategy development
- Value and cost projection
- Member risk adjustment gap identification
- Provider performance education and reporting
- Performance management reporting
Advantasure recommends bundling its risk adjustment program with administrative and care management solutions to experience comprehensive success.

Advantmed
Advantmed offers end-to-end risk adjustment solutions with 98% coding accuracy to provide accurate risk profiles for enhanced results. Here’s an overview of its risk adjustment services:
- Advanced analytics
- Medical record retrieval
- Medical record coding
- Claims and data validation
- Health assessments
With Advantmed, providers can access understandable, actionable analytics that improve Risk Adjustment Factor (RAF) scores to close documentation gaps and utilize prevention and predictive modeling.

Apixio
Apixio is an AI-powered technology that increases risk adjustment accuracy and efficiency to decrease administrative time and cost. The platform’s risk adjustment coding and auditing solutions help teams scale chart review processes and capture complete pictures of patient population health. Apixio’s core risk adjustment services include:
- Retrospective risk adjustment
- Prospective and concurrent risk adjustment
- AI-as-a-service for retrospective risk adjustment
- AI-as-a-service for prospective risk adjustment
Equipped with these features, Apixio eases the coding workload and decreases the chart review process time without sacrificing coding accuracy.

Change Healthcare
Change Healthcare’s comprehensive risk adjustment platform, Risk View, helps healthcare insurers understand risk score trends and opportunities, optimize financial results, and identify targets for appropriate risk-adjusted reimbursement. Its risk adjustment solutions include:
- Risk adjustment software and strategy tools
- Targeted advanced risk analytics
- Risk adjustment activity management
- Standardized and customized reports and dashboards
Change Healthcare offers comprehensive reports to inform strategic planning based on end-of-year and end-of-project metrics. Models used AI, big data, and chart selection to assess and target appropriate members.

Cotiviti
Cotiviti’s risk adjustment solutions ensure compliant, accurate compensation for member risk burdens. The platform provides advanced tools to optimize risk-associated revenue while maintaining transparency at every stage of the process with the following services:
- Suspect analytics
- Medical record retrieval
- Medical record coding
Cotiviti also recently acquired Edifecs, a big name in healthcare interoperability. This acquisition combines Cotiviti’s innovative health technologies with Edifecs’s data exchange capabilities, furthering their shared mission to drive advancements in health data analytics.

Episource Clarity Platform
The Episource Clarity platform is an end-to-end solution for risk adjustment and quality initiatives built to deliver tangible outcomes for leading health plans and risk-bearing providers. The platform portal includes the following applications:
- RAF analytics and suspecting tools
- Data acquisition services
- NLP-powered medical chart coding
- Clinical support including provider engagement and pre-visit review
- EDI data submission
Intending to “provide clarity at every stage,” the Episource Clarity Platform supports care teams by identifying areas of opportunity, assessing program performance, and providing comprehensive compliance review.

Pareto
Pareto’s risk adjustment solution, Pareto Hub, is a cloud-based data environment built by business experts that transforms and enriches raw, disparate data assets into business-ready analytics. The solution’s core capabilities include:
- RADV mock audit and support
- Program evaluation and strategy
- Compliance risk assessments
- Coding services
- Medical coding compliance evaluations
- In-home assessments
- Virtual home visits
- Advisory services
Pareto’s Data Management Platform enables data ingestion of all formats and types at scale with built-in governance mechanisms that maintain compliance and efficiency.

Vatica
Vatica’s solution takes a unique approach to risk adjustment — combining comprehensive data and health technology with expert clinicians at the point of care. Its provider-centric approach places PCPs at the center of interventions through capabilities such as:
- Actionable, automated provider alerts
- Intuitive coding and documentation
- Automatic transmission of accepted diagnosis codes to the EMR
Vatica receives feedback and insights from its physician advisory board, which is comprised of active Vatica clients who know the needs that providers face firsthand.
Datavant
Datavant is a data connectivity solution that helps health plans turn members’ health records into valuable assets for risk adjustment. This provider enables intelligent data exchange by linking:
- Proprietary data: Pharma trials data, social determinant data, etc.
- Third-party data: Lab data, claims data, etc.
Datavant has also partnered with Arcadia to help organizations connect Arcadia’s vast data sources with other types of real-world data.

Signify Health
Signify Health takes its risk adjustment offerings to the frontlines of patient care by facilitating in-home health evaluations and preventive services. By bringing risk adjustment to patients’ doorsteps, this vendor helps health teams connect with members and better understand patients’ current health status through:
- Medical history analysis
- Physical examination
- Medication review
- Preventive screenings
These evaluations support accurate clinical documentation for appropriate reimbursement.

Optum
Optum is a big name in healthcare analytics, delivering risk adjustment software that emphasizes RAF accuracy and documentation quality. Their full suite of solutions includes:
- Analytics consulting
- Medicaid risk adjustment and quality
- Member engagement solutions
- Prospective solutions
- Quality solutions
- Retrospective solutions
- Risk view
Additionally, Optum provides a community where health professionals can connect, discuss questions, and share resources to improve their risk adjustment approaches collaboratively.

Reveleer
Reveleer is another player in the risk adjustment game that is leveraging AI to transform HCC capture and RAF accuracy. This solution boasts up to 99% accuracy in identifying potential missed diagnoses, as well as beneficial features like:
- CMS and HIPAA-compliant workflows
- Advanced medical record retrieval
- Early CMS and RADV-IVA submissions
- Real-time dashboards to monitor coding accuracy
- Chase prioritization, suppression, quick clinical review, and one-click validation
With Reveleer’s platform, health teams can improve reimbursement accuracy by predicting future revenue adjustments and surfacing missed opportunities.

Persivia
Persivia offers AI-driven risk adjustment software that supplements accurate medical record documentation with the power of unstructured data for more point-of-care insights. This solution’s top features include:
- Real-time data aggregation
- Coding opportunity identification
- Risk analytics
- Care management tools
- Provider engagement
By delivering valuable insights such as care gaps and HCC scores to the provider at the point of care, Persivia’s solution empowers informed decision-making and increased provider satisfaction.

Inovalon
Inovalon’s SaaS suite of solutions encompasses various aspects of health plans’ efforts to manage and improve health outcomes. Primarily, its risk adjustment software delivers real-time analytics for prospective and retrospective gap identification. Its tools include:
- Risk score accuracy software
- Converged risk surveillance analytics
- Converged patient assessment
- Healthcare data lake
- Electronic record on demand
- Converged submissions
Inovalon’s cloud-based approach to analytics also supports scalable health programs, making it a great option for large-scale health plan management.
Final thoughts on risk adjustment software
Accurate risk adjustment requires several moving parts to work simultaneously, including data collection and analysis, standardization, predictive modeling, and continuous monitoring. A robust software solution can automate many of these processes, resulting in enhanced collaboration, accurate reimbursement, and improved patient care.