What conditions are causing hospital readmissions?
When it comes to healthcare, everybody wants an easy resolution. Here, we look at data on what conditions have the highest hospital readmission rates in the US.
The old adage says that an apple a day keeps the doctor away. If only staying healthy was so simple (…and cost-effective).
In an effort to understand which chronic conditions prompt the most readmissions at hospitals across the country, Senior Manager of Customer Insights Dan Sweany and his fellow team members delved into data. What they found leads to important questions around hard-to-tackle diseases, from the cost of care — readmissions are expensive — to where resources might go furthest. Read on to learn more about which conditions are sending patients back into hospital beds, and to discover more about how data can lead to action.
ICD-10 codes and diagnostic data
To conduct this pull, the Customer Insights team used data from 2021 MSSP plans to assess several tiers of ICD-10 codes, a standard way for providers to catalog and mark patients’ conditions. Starting with larger categories — like "diseases of the circulatory system" — these can be broken down into more precise criterion, like vascular disease or essential hypertension.
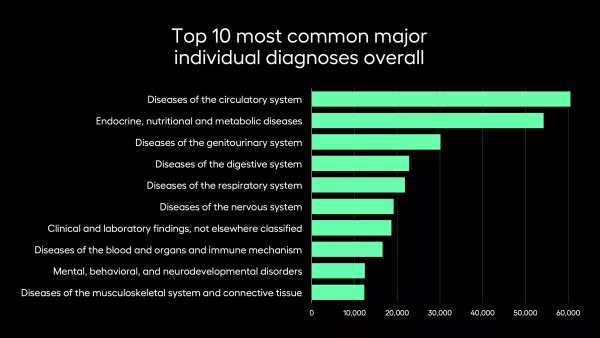
Sweany and his team found that diseases of the circulatory system account for the majority of readmits, followed closely by endocrine, nutritional, and metabolic diseases. The least frequent category for readmissions that made this chart is conditions originating in the perinatal period.
In practice, this looks like grouping a lot of what might bring people into a hospital’s waiting room into large clusters. Each category contains numerous potential diagnoses, so an elderly man with a conduction disorder and a twenty year old woman with a cardiac dysrhythmia would be in the same category.
But knowing whether the lion’s share of sick patients suffer from one particular disease or another matters a lot when it comes time to care for a large population. To drill even further into these meaningful distinctions, let’s look at the minor diagnoses (the actual conditions that can be attributed under these broader categories).
The main readmissions culprits: endocrine and circulatory disorders
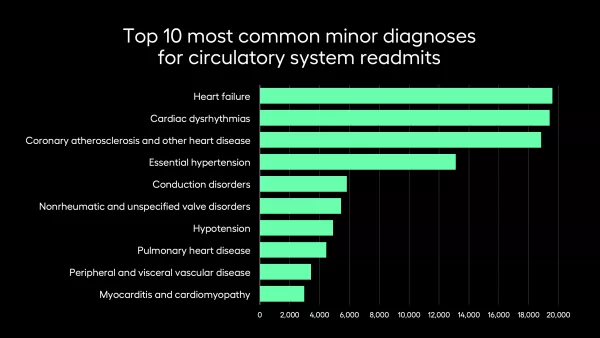
Heart failure emerged as the top circulatory disease prompting hospital readmits. This tracks with the data and studies that already exist — heart failure is a complicated, difficult-to-treat problem that afflicts many Americans. In another data pull the team undertook, heart failure also proved to vary significantly region-by-region.
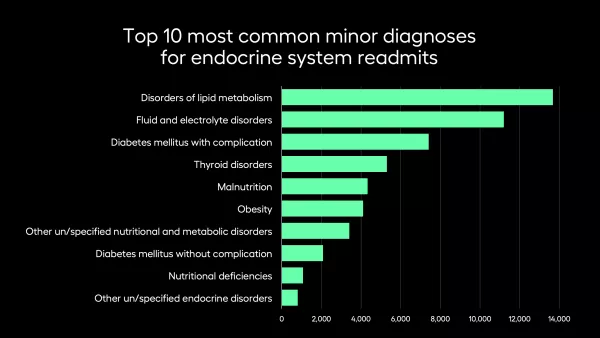
In the case of endocrine disorders, disorders of lipid metabolism proved most likely to result in readmissions. Though it’s more specific than “there’s an endocrine problem,” it covers a few common conditions, most commonly LDL-hypercholesterolemia, hypertriglyceridemia, mixed hyperlipoproteinemia, and low HDL cholesterol.
“In the emergency department, we have a specific diagnosis code of pure hyperglycemia,” Sweany says. “Each diagnosis code is placed into a hierarchy that allows us to more easily classify each distinct code. In this case, the broader 'major’ category classifies this code as an endochrine issue. Then, we can use the ‘minor’ classification to specify the specific type of endochrine issue, in this case it is a disorder of the lipid metabolism.”
Like many of the issues represented in these findings, one issue doesn’t exist in a vacuum from the others. Diabetes, for example, can exacerbate a lipid disorder, while high blood pressure can cause heart failure.
Key diagnoses that send people back to the hospital
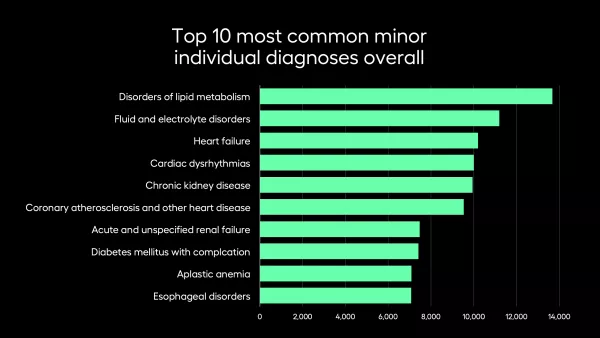
When the Customer Insights team looked at the data without the umbrella categories, the top readmission diagnoses were a diverse mix between the different systems, from endocrine to respiratory.
In this alternate view, disorders of lipid metabolism remains at the top, but the five most likely reasons for readmission are diverse. Kidney disease might not slot neatly into either category, but this graph shows what a major impact it can have on populations.
If a healthcare organization is looking to figure out where an intervention might help the most people, it would probably make sense to consider both graphs. If circulatory issues are the largest concern, does it make more sense to put those at risk of heart failure in a care management program, or are funds better spent providing free screening services to those with hypertension? The larger categories can misconstrue reality — that, despite their similar relationship to a bodily system, these conditions all require different approaches and interventions.
Volume vs. rates in hospital readmissions
An important consideration in this data is the different between volume and rates.
There are conditions with high rates of readmission that may or may not be represented in these statistics, simply because of the variance in how many people are impacted. For example: with a large population of diabetics, even a small percentage of readmissions will probably skew the numbers, whereas a rare neurological condition with a high readmission rate might not even register on these graphs.
“Since few people have, for instance, brain tumors, you're not going to have as many readmits for those patients,” Sweany explains by way of example. “The readmit rate might be 100%, but since the volume is so low, you won’t see those diagnoses topping the charts here."
In short, it’s important to take a critical eye to this (and all) data. It won’t tell you which conditions are most fatal, or which conditions require the most readmissions in general. This shows, instead, the largest groups, and leans towards diseases that a vast amount of Americans share.
The data you need for the insights that matter
The first step to creating effective population health interventions is knowing that population, from the big picture to a granular level.
Learn more about the data Arcadia’s Customer Insights team is surfacing, and discover how data analytics can sharpen your view for the healthcare challenges ahead.
