How interoperability streamlines CMS reporting
A shifting CMS landscape means healthcare organizations must constantly update their technology and reporting processes. Learn how interoperability can enhance the volume and quality of data and improve quality of care.
Medicare reporting requirements change regularly, and as a result, healthcare organizations have to update their own workflows and reporting processes in accordance. As technology progresses, so do CMS’s requirements.
A January ruling strengthened requirements for Health Information Exchanges (HIEs) and made the prior authorization process more transparent. Additionally, the industry and governmental bodies continue to tighten standards around trusted exchange frameworks (through acts like TEFCA). This means partner organizations will need to implement new technology and provisions to comply by January 2026.
Arcadia Director of Enterprise Partnerships Andrea Purjue recently spoke with Charles Spence, Cigna’s Senior Director of IT Strategy, Government Business Segment about how this is impacting healthcare organizations. Read on to learn how you can leverage technology and update workflows to reach compliance without slowing down existing processes.
Why interoperability matters in healthcare
Updated information requirements are really a data management issue — if CMS needs more thorough or granular data, healthcare organizations need a firm grasp on data collection, storage, and sharing. This is where interoperability comes in.
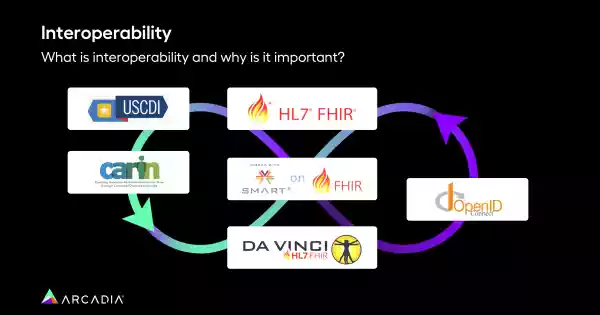
Interoperability is the ability for information to flow unimpeded across different applications, platforms, or devices, so that it is exchanged between an organization’s users without lags or degradation of the data itself. For an interoperable system to function well, it also needs to be secure. Many different data structures can be interoperable, from the wheel-and-spoke model of a zero-copy data lake to the more traditional point-to-point or mesh architecture.
How interoperability streamlines CMS reporting
When it comes to CMS, “It’s really about getting the data to the customer or your beneficiary at the right point in time,” says Spence. “What’s their data need for care management, for example? How do you share that journey of care coordination with providers?”
Interoperability can help break down information silos and lead to whole-person care. It also facilitates patient engagement. Interoperable systems can provide patients with easier access to their health information, enabling them to take a more active role in their health and care. This can lead to better compliance with treatment plans, more informed healthcare decisions, and improved communication between patients and healthcare providers.
In an interoperable system like a healthcare data analytics platform, a provider can see a patient’s entire history (not just an incomplete slice of their records). When the average hospital deals with 18+ EHRs, this fluid yet secure transfer of information is a crucial part of delivering quality care — and providing CMS with the detailed, well-documented records they require.
Building an interoperable healthcare system
“It’s a lot more complicated than just saying, ‘Hey, go out and get interoperability stood up.’ It’s about how you do it, and how you effectuate it,” Spence says. “If you can’t integrate the data into [an organization’s] respective EMR or their platform, what good does it do?”
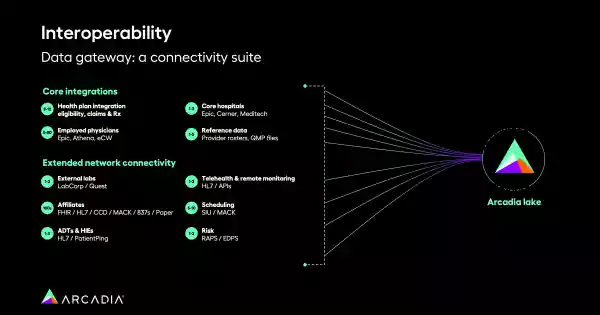
Payer data forms the foundation of any arrangement in value-based care, but any healthcare organization benefits from an easily accessible, vast pool of data sources. A data platform is an optimal solution to this challenge, integrating data from hundreds of sources, like external lab results and ADTs.
From there, it’s about synthesizing this information so it’s useful.
“We have so much data — claims data, different types of medical data,” Spence says. “How do you get all that abstracted to be something of use that’s meaningful?”
A healthcare data analytics platform lets organizations stratify that data into meaningful groupings, driving increased ROI. Patient stratification lets care managers identify precisely who’s eligible and most likely to benefit from a diabetes nutrition program, for example, offering a granular view of health through a history of ICD codes, ED visits, and more. It can also track spending, so that healthcare organizations can see where the majority of their resources are going (and report that to CMS for reimbursement).
Report to CMS with confidence
CMS guidelines are always shifting. As Spence puts it, healthcare organizations are constantly “changing the tires on a moving vehicle.”
Knowledge is power, and the more detailed picture a healthcare organization has of their patients and populations, the better they can convey their work to CMS and claim the payments they’re owed. With great interoperable tech, this wealth of insights is available and easy to share, whether that’s between teams or to an outside party.
Watch Spence and Purjue’s full discussion to learn how Arcadia can be your partner in progress.
