One Source Isn’t Enough: Why Data Aggregation Is a Strategic Imperative for Payers
Data is at the core of nearly every payer strategy, from care management and quality measurement to member engagement, population health, and equity initiatives. Whether designing targeted programs, evaluating outcomes, or fulfilling regulatory reporting requirements, payers need data that is complete, timely, and accurate.
Yet, payers are often limited by the quality and completeness of their data, especially when relying solely on either claims or clinical sources. Despite 96% of payers recently surveyed by Arcadia saying they maintain longitudinal member profiles, 85% of the payers we surveyed reported that they hadn’t integrated all the data in their ecosystem. Moreover, 39% stated they had difficulty aggregating clinical and claims data.
The insights reveal discrepancies between payers’ perceived data aggregation capabilities and the current reality. Without enabling data-driven strategies that support better care delivery, payers may be missing opportunities for performance improvement.
Aggregated Data = Better Member Identification
Each stream of data that a payer can access offers important, but incomplete insight. Claims data captures utilization and costs, while clinical data adds necessary detail on diagnoses, lab results, and member-reported factors.
To drive performance across strategic initiatives, payers must integrate all available data sources to create a complete picture of each member. This aggregated view, referred to as a member 360—a comprehensive, longitudinal profile combining clinical, claims, and supplemental data—is what enables smarter decisions, more equitable care, and better outcomes.
This is evident using the example of care management, where success depends on the ability to accurately identify and engage the right members at the right time. Without a holistic understanding of the member, payers risk missing those who are most in need of support or targeting those who are unlikely to benefit.
To illustrate this point, consider a recent analysis conducted by Arcadia comparing three approaches to identifying high-risk maternity members for a care management program:
- Claims data alone identified 837 members
- Clinical data alone identified 1,080 members
- Aggregating both claims and clinical data identified 1,213 members
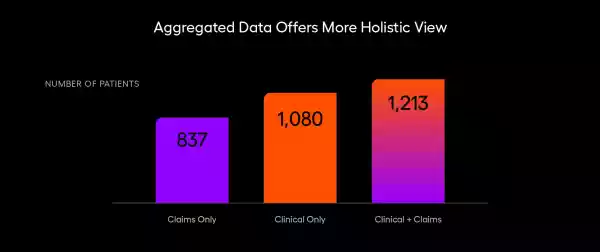
This analysis demonstrates that combining both data sources identifies more high-risk members than either source alone. When claims data is added to clinical data, identification increases by 12.3%. When clinical data is added to claims data, identification improves by a dramatic 46.7%
From Data Aggregation to Better Outcomes
Payers relying on a single data source are limited in the accuracy, completeness, and effectiveness of any strategies that rely on data, which underpin today’s payer priorities — including risk assessment accuracy (identified by 54% of payer leaders as a priority), expanding members (a priority for 45% of executives we surveyed), and network performance (a priority important to 39% of payers).
Fortunately, when a payer aggregates clinical and claims data, it strengthens every downstream function:
- Stratification: Data-rich risk models can better differentiate between high-risk members and impactable members, enabling management of the right member at the right time in their care trajectory to optimize limited resources.
- Engagement: Insights from EHRs can drive personalized outreach—for example, by addressing language barriers or social needs.
- Measurement: Aggregated data improves the accuracy of quality and outcomes reporting across lines of business.

If you’re only relying on a single source of data instead of accessing and aggregating all of the data you have access to, you’ll be limited in your accuracy, completeness, and effectiveness.
What Can Payers Do Today?
Many health plans already have access to clinical data through value-based contracts, interoperability frameworks, or partnerships with provider networks. But access alone isn’t enough. What matters is integration, normalization, and intelligent use.
Here’s a starting point for action:
- Invest in aggregation infrastructure: Work with analytics platforms or partners that can ingest and normalize multiple data types at scale.
- Integrate into care workflows: Ensure care management teams can easily access aggregated views, not just raw feeds.
- Monitor equity impact: Use aggregated data to track disparities in identification, engagement, and outcomes, and adjust interventions accordingly.
The success of any payer program depends on engaging the right members at the right time. Aggregating data across claims, clinical, and supplemental sources is no longer a “nice to have”—it’s a foundational requirement for precision, impact, and equity.
As payers continue to evolve toward whole-person, value-based care, the organizations that unify their data will be best positioned to serve their members effectively and measurably improve outcomes.
