Improve efficiency and meet patients’ needs with a care management program backed by data
Care management programs involve multiple moving parts, from setting strategy to managing spend to improving outcomes. How you monitor and prioritize these pieces is key to keeping your program lean and efficient. Your current data solution is critical to balancing the best possible care with waste-reducing business intelligence.
The Challenge
Care management is an important component of population health management, but healthcare organizations sometimes struggle to assess the impact and maximize the value of a given program. Poor measurement strategies can result in organizations cutting their care management programs too early, before they have a chance to show results. Poor measurement can also cause a misalignment between the resources being invested and the organization’s ultimate population health goals.
The Solution
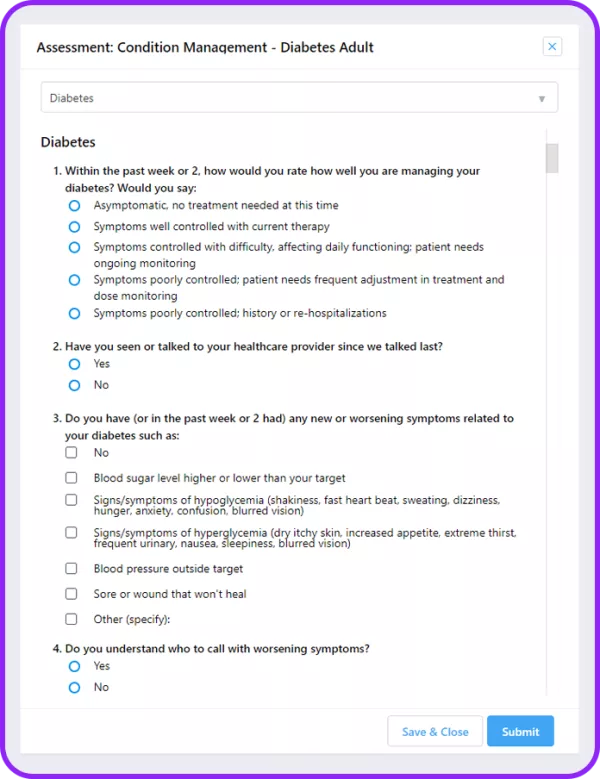
Equip your team with robust data and predictive analytics through every step of the care journey. When you leverage Arcadia’s aggregation and analytics to determine next steps, you can break down silos and take informed, productive action. Take advantage of algorithms that present simplified identification and stratification, plus dynamic cohorts, updated in real time. Finally, recoup more time, allowing care managers to focus on what matters most: matching patients to interventions.

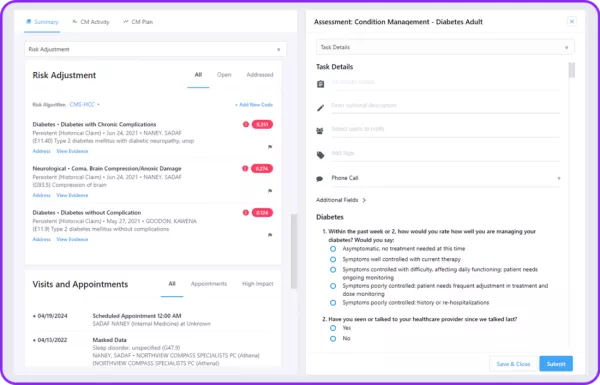
Identify patients with the most need and highest impact
- Drill deep into patient histories to find specific, eligible populations
- Equip team members with care management dashboards that identify risk factors and address health concerns early in the process
- Create nuanced, specific programs with attainable goals based on demographic insights
Estimate cost and potential savings to allocate resources efficiently
- Match potential cases with care managers, social workers, and other members of your team to manage caseloads and identify staffing needs
- Leverage predictive analytics to see who’s most at risk and stop issues before they start
- Stratify impacted populations so outreach is tailored and impactful, increasing enrollment
Measure impact and refine processes
- Combine case control and retrospective review to get a holistic sense of what works (and what didn’t)
- Easily share and communicate results with key stakeholders
- Assess impacts at regular, automated intervals, so you can refine as you go
Strengthen care management programs with data and predictive analytics
Leverage Arcadia’s care management offerings to turbocharge your analytics. From population identification through outreach, simplify the process of matching the right patients to the right interventions. Tap the Arcadia insights you know and rely on, now empowering your care managers.
What happened when our partners incorporated Arcadia’s Care Management tools:
- A Northeast ACO had a 41.5% reduction in ED visits for COPD patients
- A multi-state ACO reduced treat-and-release ED visits 365K to 296K
- Another Northeast ACO served 3x more patients with the same care management team
Maximize your care management team’s impact while refining efficiency, so you’ve got a future-proofed, industry-leading program that helps patients today and equips them for tomorrow.
Arcadia can help turbocharge your care management.
Contact us today for a no-obligation demonstration.
