The power of HPV vaccination for cancer prevention strategies
Without vaccination, almost every sexually active person on earth will get HPV (human papillomavirus) in their lifetime. The virus is now known to be the culprit of many cancers. Therefore, reducing the number of people who get HPV is a strong cancer prevention strategy.
A vaccine against HPV was first approved in 2006 and by 2019, more than 100 countries had added it to their regular vaccine schedules. The HPV vaccine is the only cancer prevention vaccine in existence today. With that power, it would be easy to believe there would be high demand for it. However, HPV vaccination rates lag behind most other adolescent vaccines and rates are lower for adults.
Dr. Kate Behan, Chief Medical Officer at Arcadia led a discussion with Dr. Thomas Schuch, Chief Information Officer, South Boston Community Health Center, Dr. Jay Lee, Medical Director at Integrated Health Partners of Southern California, and Dr. Daniel Faden, Assistant Professor in the Department of Otolaryngology at Harvard Medical School who offered their insights on addressing this important population health issue in a recent webinar.
HPV causes many types of cancers
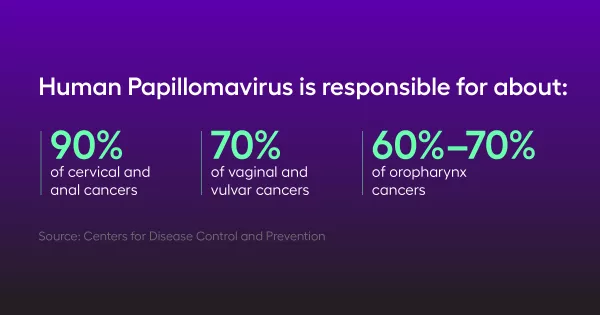
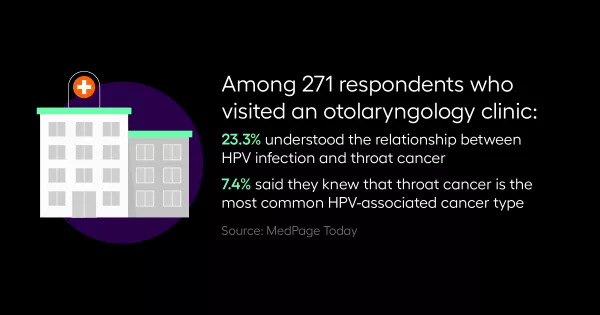
The link was first made between HPV and cervical cancer, but additional research in the past decade has uncovered links between the virus and anal, vaginal, and oropharynx (cancers in the back of the throat) cancers as well. Head neck surgical oncologists like Dr. Faden are seeing very high rates of oropharynx cancers caused by HPV.
“About 10 years ago, oropharynx cancer surpassed cervical cancer as the most common HPV associated cancer in the U.S.,” he said.
Knowing that HPV is responsible for so many types of cancers should change the thinking about vaccination, but among many patients and health providers, the focus remains on cervical cancer. Healthcare experts are working hard to change the idea that only women or teenage girls should be vaccinated to include everyone.
Addressing barriers to vaccination
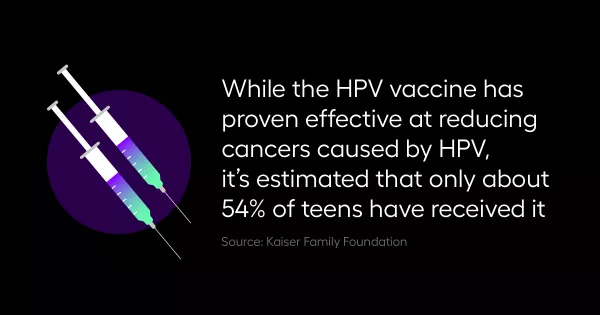
In the U.S., the vaccine is recommended to be given at age 11 or 12 and up to age 45. However, HPV vaccination lags behind other adolescent vaccines with only about 54% of teenagers vaccinated.
The most powerful way to increase those numbers is through trusted provider-patient relationships that can overcome three common barriers:
1. Vaccination guidelines have changed: Since the vaccine’s release, the guidelines for its use have changed, causing confusion among both patients and providers. Education about HPV, when to start giving the vaccine, and who to give it can help overcome the idea that this vaccine is optional and combat the low vaccination rate.
“We need to train providers to think about HPV first, because this is a prevention vaccine and we need to get it early,” Dr. Schuch explained.
2. Misconceptions among parents: Many parents worry that giving their child this vaccine will encourage sexual activity at an early age based on information that they got off the internet, or rumors that they may have heard from co-workers or family members. Dr. Lee says that parents need to know that this vaccine prevents many types of cancers and that patients must receive it before they are in a position to contract HPV. He believes shared decision making can be a helpful strategy for physicians making the case.
3. Lack of access or interaction with the healthcare system: Young men have few reasons to interact with the healthcare system unless they have some acute problem, unlike women who regularly see a gynecologist, making the opportunities to vaccinate less frequent. Dr. Schuch points out that because many adolescents don’t make routine visits after age 11 or 12, making any visit an opportunity to educate patients about vaccines is critical.
“Turn on the preventive care reminders to start at nine and make care alerts so that when they come in with a sore throat you have an opportunity to do whole person health and bring up the vaccine,” he explained.
Data and technology’s role in robust vaccination programs
Healthcare organizations need to prioritize investments in data analytics. Tracking data metrics is the only way to know where you are related to your goals.
Dr. Schuch says healthcare organizations should have a process metric to know how many HPV vaccines they’re giving in a week or a month; what ages they are giving them at; and the age of completion.

“Looking for an outcome metric is going to take a longer time, but you can set yourself up for quick wins by looking at the process metric for whatever strategy you implement,” he explained.
Monitoring effectiveness means bringing data to the point of care. Getting data fluency helps clinical teams when they have the patient in front of them, because data can inform that patient-clinician encounter.
A true cancer prevention strategy
HPV associated cancers are five percent of all cancers. Five percent of all cancers are preventable with this vaccine.
“This is a life and death question — this is a cancer preventing vaccine; the only one that we have right now,” said Dr. Faden. “If people can understand the immense impact of these cancers. The ability to prevent that can't be overstated.”
Watch the full webinar to learn more about HPV vaccination efforts. Please reach out for details and a demo of Arcadia’s healthcare data analytics capabilities.