What you should know about SDoH and SOGI, the data sources shaping health equity
Health disparities are some of the greatest drivers of inequity. Whether it’s lack of access to care or stigma that prevents a patient from receiving the care they need, no one walks into a hospital as a blank slate — our identities and histories affect our health. Two acronyms cover some of the most high-impact factors driving these inequities: SDoH (social drivers of health) and SOGI (sexual orientation and gender identity).
If the status of someone’s health is a mosaic of lab results, lived experiences, and numbers on a chart, a healthcare organization won’t have the full picture unless they incorporate all this data.
Nick Daniel, Director of Product at Arcadia, recently discussed why this data is a crucial weapon in the fight against health inequity and how technology can help healthcare win this battle. Read on to learn why these two data sources are so important to healthcare's mission.
What are SDoH and SOGI?
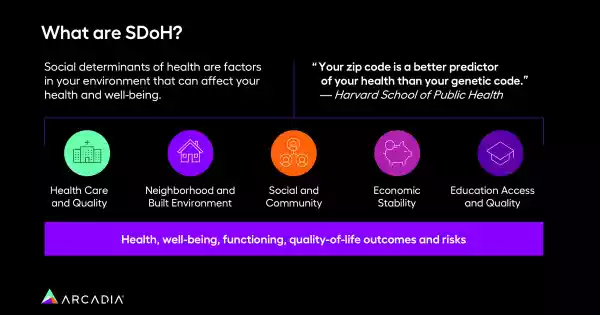
Social Drivers of Health (SDoH) refer to the conditions in which people are born, grow, live, work, and age. These factors can include:
- Socioeconomic status
- Education
- Neighborhood and physical environment
- Employment
- Social support networks
- Access to healthcare
SDoH are instrumental in shaping the health of individuals and communities, often predicting health outcomes more accurately than genetic predispositions.

Sexual Orientation and Gender Identity (SOGI) data refer to an individual’s self-reported sexual orientation and gender identity. The collection of SOGI data is vital for identifying the unique health needs of LGBTQ+ communities, who often face significant health disparities and barriers to accessing healthcare services.
Why documenting SDoH and SOGI matters
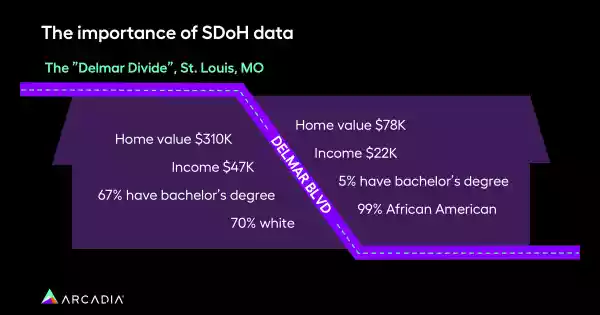
A patient’s zip code is a better predictor of health than their genetic code. Documenting SDoH and SOGI is essential for developing targeted interventions that address health disparities. In short: to take the temperature of any population, you need data.
Arcadia's insights team discovered that members living in areas with higher rates of SDoH impact go to the emergency department 20% more frequently and have 24% more avoidable ED visits. These same members require an inpatient stay 15% more often.
Documenting these factors allows healthcare organizations to tailor and understand their population’s needs, but it also allows them to reduce their per member per month (PMPM) costs, which are 5% higher on average for patients in areas highly impacted by SDoH factors.
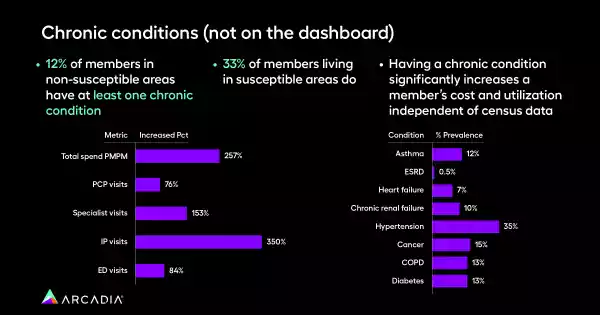
Unique demographics also face unique health challenges. Capturing that demographic data can reveal other meaningful insights. For example, 33% of members in susceptible areas also have at least one chronic condition compared to 12% in non-susceptible areas.
Recent data collected by Arcadia also shows that chronic conditions, which are higher in areas susceptible to SDoH factors, come with a steep cost for healthcare organizations — the total PMPM spend for someone with a chronic illness is 257% higher than a patient without. A social intervention that tackles housing insecurity, for example, might be the key to reducing hypertension in a population.
The team also pulled average increases across several cost/utilization categories, payer categories, and census concepts to see which factors drive increases. The largest determinant of increased cost/utilization is the metric that determines whether a member is considered below poverty line, but the others show similar splits:
- 30% more avoidable visits
- 27% more ED visits
- 12% more IP visits
- 10% more PMPM
- 4% more PCP visits
- 5% fewer specialty visits
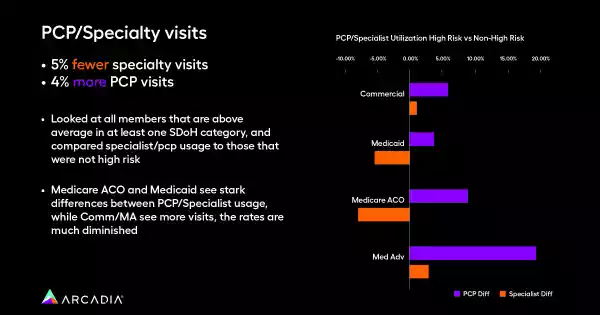
Furthermore, data shows a major discrepancy in PCP versus specialist visits for populations greatly impacted by SDoH. Patients identified as part of these demographics saw specialists 5% less frequently than their unimpacted counterparts, yet visited a PCP 4% more often. Though the cause for this isn’t immediately clear, there are a number of reasons this could be — availability of specialist doctors in particular regions or areas, lack of awareness about these niche providers, or less time to navigate the bureaucratic red tape necessary to get a referral.
With this knowledge at their disposal, healthcare organizations can encourage more specialist interventions within certain populations (like street clinics for screenings or bilingual literature advertising available care). Providers at these organizations can also receive training on referrals and gathering additional social data.
Challenges in data integration for SDoH and SOGI data
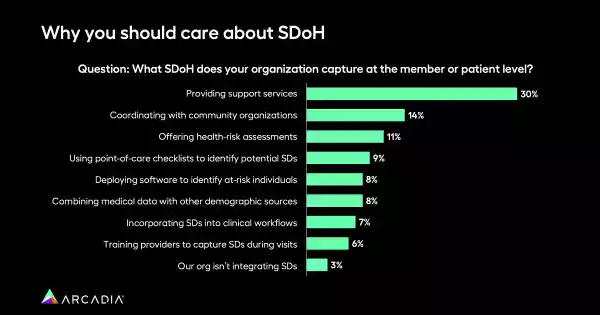
Integrating and working with SDoH and SOGI data is not without challenges. One major issue is data capture. Many healthcare providers are hesitant to ask patients about their sexual orientation and gender identity due to fears of offending them — despite studies showing that a significant majority of patients are open to sharing this information.
Social stigma also plays a prominent role, because some patients are hesitant to share challenges like housing insecurity or financial struggles with providers. Facing this barrier head-on is crucial for building better systems.

By capturing the data, it really opens the door for a more trusting, open, and honest patient-provider relationship. It's not something we have to dance around — the provider can have this information going in, so the provider is not saying the wrong pronouns, or making the wrong assumptions about a person. In turn, that makes the patient feel more comfortable, and more willing to seek treatment and care when they need it.
The healthcare sector also faces challenges related to inconsistencies in terminologies and codes for these data types. A lack of standardization can make it difficult to analyze datasets since there are many ways to describe the same phenomena. Additionally, the sensitive nature of SOGI data raises concerns about privacy and security, adding layers of complexity to data management.
Technological solutions to SDoH and SOGI data challenges
Healthcare technology platforms are one of the most powerful tools healthcare organizations have for combatting the effects of SDoH and SOGI disparities.
Data analytics facilitates the integration of data from many sources, providing a more comprehensive view of the social factors influencing health. Features like interoperability and a hub-and-spoke architecture let healthcare organizations:
- Share data easily across different systems
- Enhance access and cross-departmental communication
- Facilitate easy data sharing and coordination between different teams and providers
- Segment patients for effective care management
- Outreach to patients via automated text messaging
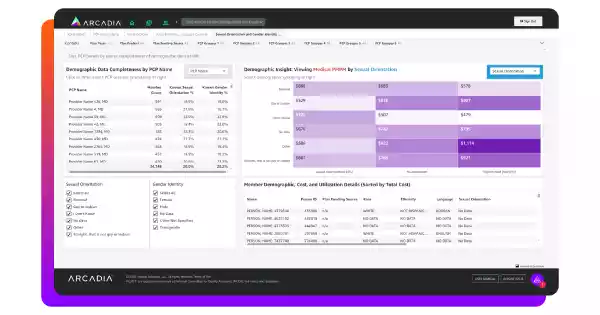
Critically, Arcadia’s Health Equity dashboard also puts social factors into financial perspective. With a tool dedicated to the impact of SDoH, healthcare organizations can prevent unnecessary ED visits, shorten inpatient stays, and target high-cost chronic conditions.
Extend and improve lives, no matter the barriers
When it comes to SDoH and SOGI, the first step is simply gathering the right information at the right scale. By learning and addressing the unique health needs of various communities, healthcare providers can extend and improve the quality of life for individual patients and large populations alike.
Armed with the right tools, healthcare organizations can wield technology to level the playing field, promoting more inclusive and equitable healthcare for all. Discover how data analytics can help you advance better health.
