Strategic provider attribution: Enhancing patient-to-provider alignment in population health
Provider attribution in healthcare is vital for managing population health and achieving value-based care goals. In Arcadia’s byte-sized insight series, Julia Kelly, Director of Application Enablement, explores its intricacies and how organizations can align their strategies with overarching healthcare objectives.
Provider attribution in healthcare: Uncovering its components
Provider attribution defines the relationships between patients and providers. It uses a data-driven approach to determine which provider is responsible for a patient's care. This is done by analyzing the patient's utilization history, condition history, and various clinical and claims data points.
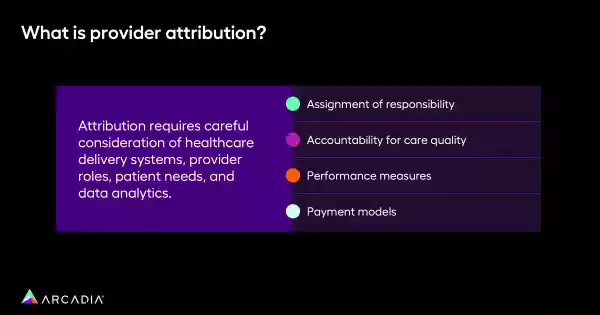
Organizations must strategically collect and synthesize data to define effective attribution. This ensures alignment with population health management and value-based care goals. Successful attribution demands careful consideration of healthcare delivery systems, provider roles, patient needs, and data analytics.
The key pillars of attribution
Understanding the core components of provider attribution is essential for healthcare organization. There are four key pillars to consider when looking at provider attribution:
1. Assignment of responsibility
Attribution involves assigning responsibility for a patient's care to a specific provider. This process is complex due to the diverse stakeholders involved, including providers, care teams, practices, hospitals, and health systems.
2. Accountability for care quality
Once a provider is assigned, they become accountable for the quality of care, which drives improvements in patient outcomes, boosts patient satisfaction, and ensures adherence to care best practices.
3. Performance measures
Provider assignments often tie to performance measures. Organizations must ensure that the selected provider aligns with the metrics and measures set to achieve success in reporting and contracting.
4. Payment Models
In value-based care models, provider performance often links to payments. Providers and facilities receive incentives based on their performance, making accurate attribution crucial for financial success.
These key pillars form the foundation of a robust attribution strategy, ensuring that providers are accurately assigned, held accountable for care quality, measured against performance standards, and fairly compensated within value-based care models. By focusing on these critical aspects, organizations can drive improvements in patient outcomes, enhance provider performance, and achieve their financial and strategic goals.
How should healthcare organizations approach attribution?
Healthcare organizations should adopt a strategic approach to provider attribution, starting with a comprehensive understanding of available data points and their priorities. “I like to think of this almost like a funnel,” said Kelly. This process involves:
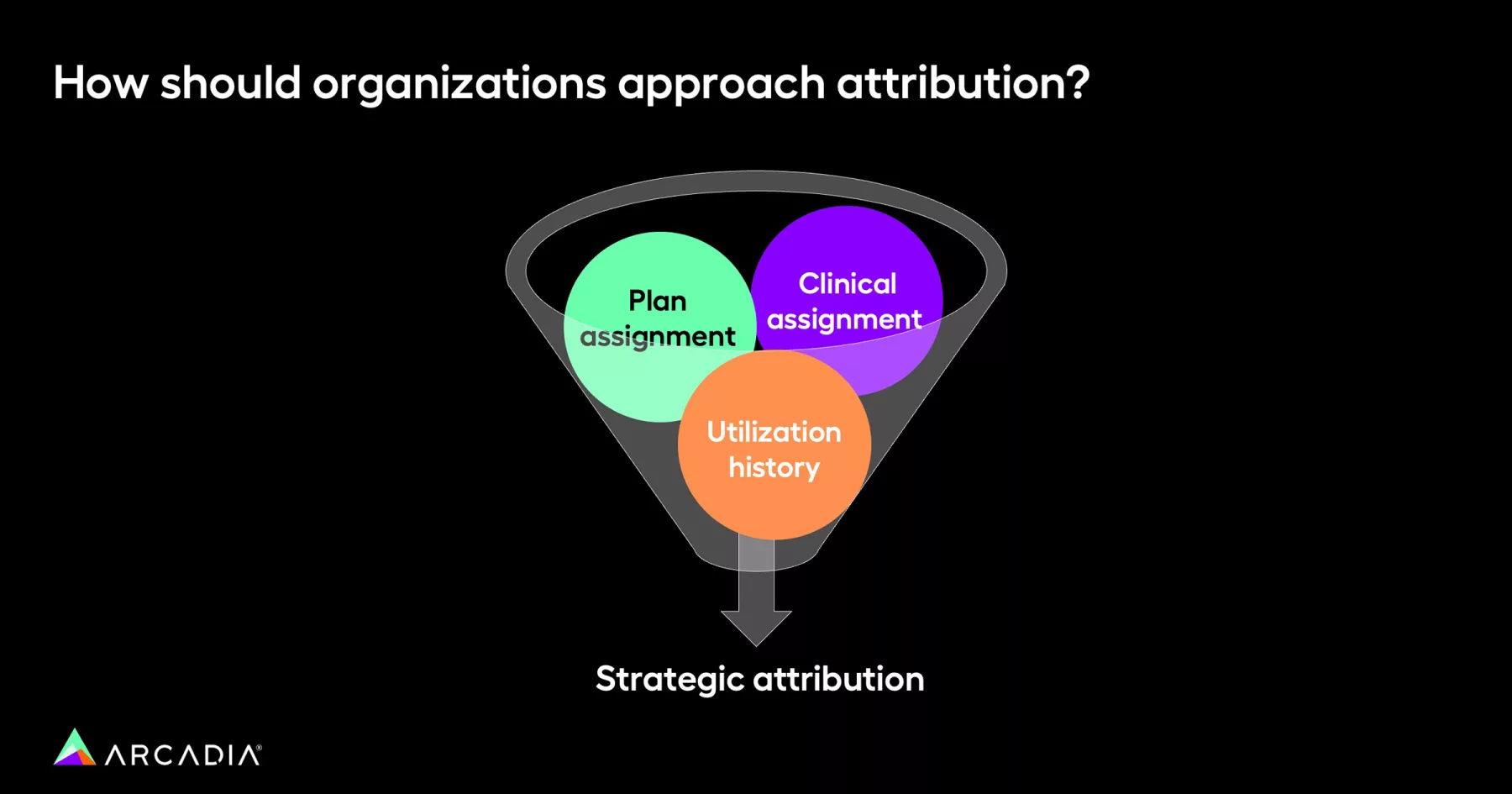
- Plan assignment: Utilize plan assignments where an external body assigns providers to patients based on data analysis. While helpful, plan assignments can be fallible and lagging.
- Clinical assignment: Leverage EHR assignments, which are typically updated in real-time. However, these can be inconsistent, particularly when patients are present in multiple EHRs.
- Utilization history: Incorporate derived assignments that consider a patient's actual utilization history, encounter data, and specific encounter types to determine the most appropriate provider assignment.
By integrating these approaches, healthcare organizations can begin to develop a more accurate and effective attribution model. This strategic alignment ensures that patients receive consistent and coordinated care, improving outcomes and enhancing satisfaction. Additionally, a well-structured attribution framework supports the goals of value-based care, driving better performance, accountability, and financial success.

At the start of an engagement, you really need to take a step back and think about what are the full scope of data points that I have available to me that are related to assignment in some way, because there are a lot.
How can organizations personalize attribution?
Organizations can enhance the accuracy and effectiveness of provider attribution by tailoring their approach to the specific needs and characteristics of their patient population. Personalizing attribution involves leveraging a combination of provider rules, plan assignments, clinical data, and utilization history. By setting clear criteria and using targeted data sources, organizations can ensure patients are matched with the most suitable providers. This criteria falls under four categories:
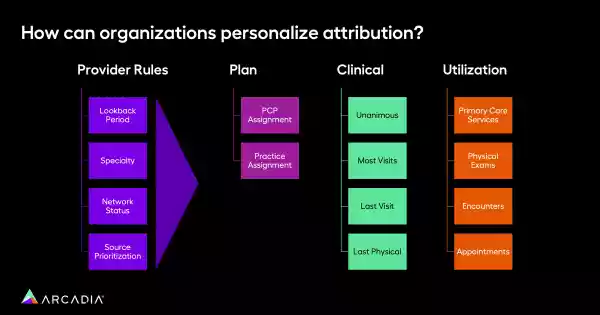
- Establish Provider Rules - Organizations can establish provider rules to filter and prioritize providers for patient assignments using:
- Lookback period: Focus on providers who have had recent encounters with the patient.
- Specialty: Limit assignments to providers rendering specific services, such as internal or family medicine.
- Network status: Assign patients to providers within a specific network.
- Source prioritization: Prioritize certain data sources over others based on their reliability and relevance.
- Plan Provider Assignment - Organizations can prioritize plan assignments at the PCP or practice level to establish a foundational source of truth.
- Use Clinical Data - Utilize clinical data to identify providers with the most visits, the most recent visit, or specific types of visits (e.g., physical exams).
- Analyze Utilization - Analyze utilization data to identify primary care services, physical exams, encounters, and appointments to inform provider assignments.
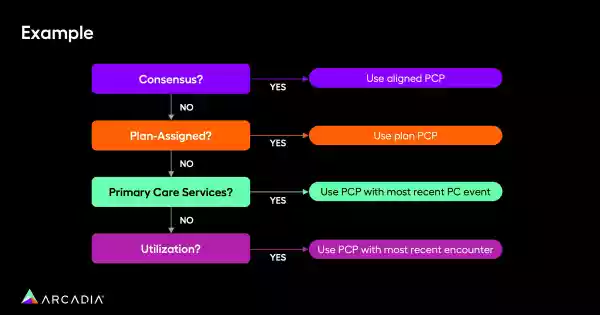
Examples of personalized attribution
An example sequence for provider attribution might involve:
- Consensus: Align with the provider agreed upon by all claims and clinical sources.
- Plan-assigned: Default to the plan-assigned provider if no consensus is reached.
- Primary care services: Consider recent primary care services to identify the most engaged provider.
- Utilization: Use encounter data to make the final assignment if other data sources are insufficient.
Achieve effective provider attribution
Provider attribution is a complex but essential process for healthcare organizations looking to improve population health and succeed in value-based care contracts. “This is not simple. A lot of different stakeholders, a lot of different data sources,” said Kelly. “But I think you really need to approach attribution with that lens of understanding: what are my priorities? How do I want to match up these people in a way that really best positions me to succeed in population health and contract performance?”
By strategically utilizing available data, organizations can accurately assign providers, enhance patient outcomes, and achieve their financial and reporting goals.
See more byte-sized insights or request a demo of Arcadia’s powerful data platform to empower your population and value-based care goals.
