Leverage technology to reshape healthcare economics: A path to improved patient outcomes
The challenges in America’s healthcare system persist, with affordable, high-quality care remaining the exception instead of the norm. Over the last decade, healthcare costs have soared, significantly impacting personal finances and national budgets.
In 2023, federal subsidies for health insurance (except certain related payments made to the federal government) are estimated to be $1.8 trillion, or 7% of gross domestic product (GDP). Healthcare expenses now rank among the leading causes of personal bankruptcy. The need for systemic changes in healthcare economics is urgent, so how can industry leaders accelerate change?
The landscape of rising costs and care disparities
In recent years, experimental strategies aimed at cost containment have been implemented, yet healthcare spending continues to rise. Factors contributing to this include surging prescription drug prices and fluctuating expenses across diverse healthcare sectors. There are new groundbreaking medications, such as GLP-1 drugs, that offer hope for better patient outcomes, but there are concerns regarding affordability, accessibility, and fair distribution.
Drug pricing disparities impacting global health systems
Beyond the United States, drug pricing disparities reverberate globally. The lobbying efforts by pharmaceutical giants to incorporate life-changing medications into Medicare Fee Schedules underscore the issue: while these drugs promise transformative benefits, achieving equitable access and sustainable funding remains a challenge.
The practice of Americans seeking cheaper medications abroad inadvertently widens healthcare disparities in countries with weaker healthcare systems, emphasizing the need for fair, accessible drug pricing strategies on a global scale.

Americans are flying to Mexico to buy in Mexico... so not only do we have health care disparities in our own communities, but we’re trampling across borders and creating health care disparities in other countries that have a much worse health care system than we do.
Leverage technology, responsibly
The escalating costs of prescription drugs prompt discussions on aligning healthcare expenses with delivered care quality. Strategies for cost reduction must converge with initiatives aimed at maximizing patient outcomes. For example, increased access to services like CT scans signifies the fine balance between widening access and prudent resource utilization.

Sometimes you had to wait three days because that was the only CT scan they had. Fast forward to 20 years later, you walk into an ED and you get a CT scan. If it’s more available, does that drive overuse of those resources? There’s a positive and a negative there.
Without strategic management and decision-making aimed toward better care, there is a risk of the overutilization of diagnostic resources and improper resource allocation. Achieving high-value care mandates careful evaluation of technological advancements' impact on healthcare economics, ensuring responsible utilization without compromising patient care quality.
While technological strides enhance affordability and accessibility, a balanced approach to resource allocation becomes crucial, prioritizing high-value care over sheer accessibility.
8 ways technology is reshaping healthcare economics
Currently, the U.S. healthcare system is leveraging various technological advancements to reduce costs and improve outcomes:
- Telemedicine and remote monitoring: Especially since the COVID-19 pandemic, there has been a significant increase in more affordable telemedicine options and remote monitoring of chronic conditions. This has reduced the need for in-person visit and travel costs, particularly in rural or underserved communities.
- Health Information Technology (IT): Electronic Health Records (EHRs) and Health Information Exchange (HIE) systems streamline data sharing among healthcare providers, reducing administrative costs and minimizing redundant tests or procedures. Interoperable health IT systems improve care coordination and enhance patient safety, leading to more efficient and cost-effective care.
- Predictive analytics and data analytics: Utilizing big data and predictive analytics helps in identifying high-risk patients, predicting disease outbreaks, and optimizing resource allocation. Data-driven insights aid in preventive care strategies, reducing emergency room visits, and better management of chronic diseases, thus lowering overall healthcare costs.
- Remote patient monitoring devices and wearables: Wearable technologies and remote patient monitoring devices enable continuous tracking of patient health metrics. These tools assist in early detection of health issues, support self-management of chronic conditions, and reduce hospital readmissions, ultimately cutting healthcare expenses.
- Generative AI and Machine Learning: AI applications streamline administrative tasks, automate processes, and enhance diagnostic accuracy. AI-powered algorithms assist in medical imaging interpretation, drug discovery, and personalized treatment plans, potentially reducing errors, optimizing treatments, and lowering healthcare costs.
- Value-based care models: Technology facilitates the transition from fee-for-service to value-based care models. These models emphasize patient outcomes over the volume of services rendered. They encourage preventive care, care coordination, and focus on population health management, thereby reducing costs associated with unnecessary procedures and hospital admissions.
- Mobile health applications and patient engagement tools: Mobile apps and patient engagement tools promote self-care, medication adherence, and lifestyle modifications. These tools empower patients to actively manage their health, potentially preventing complications and reducing healthcare utilization and associated costs.
- Robotics and automation in healthcare: Robotic-assisted surgeries, automated workflows in hospitals, and AI-driven robotics in medication management enhance efficiency, reduce errors, and optimize resource utilization, leading to cost savings in healthcare delivery.
The future of healthcare economics
The future of healthcare economics hinges on a collaborative effort to integrate technological advancements with policy reforms.

It’s a complicated picture. What I’ve seen is we’re developing a lot of technology that can reduce costs, but policy and people need to change in order to activate it.
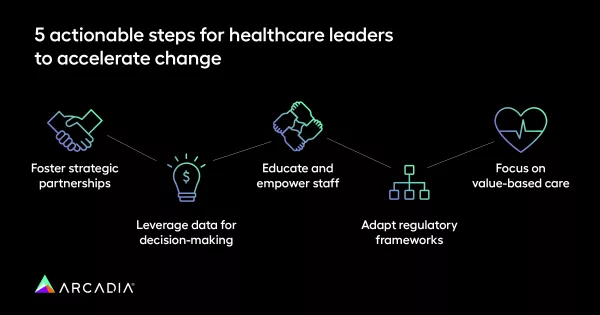
5 actionable steps for healthcare leaders to accelerate change
- Foster strategic partnerships: Collaborate with technology firms and experts to devise custom solutions addressing specific cost concerns while improving patient care.
- Leverage data for decision-making: Leverage robust data analytics to identify cost-saving opportunities and optimize resource allocation.
- Educate and empower staff: Equip healthcare professionals with the necessary training and tools to utilize technology efficiently, aligning their efforts with cost-effective care.
- Adapt regulatory frameworks: Advocate for flexible regulations to enable the seamless integration of technology without compromising patient safety or quality of care.
- Focus on value-based care: Shift the focus from solely reducing costs to emphasizing improved patient outcomes as a measure of success.
Healthcare leaders who leverage technological advancements as tools for cost containment and improved patient outcomes will play a pivotal role in shaping a more sustainable and patient-centric healthcare ecosystem.
By fostering collaborations, leveraging data, and focusing on value-based care, healthcare leaders can pave the way for a future where cost-effective care and superior patient outcomes coexist. The journey toward affordable, accessible, and high-quality healthcare begins with informed leadership and prudent utilization of technology's transformative potential.
You can check out other hot topics, in addition to healthcare economics, on Spicy Takes, Episode 1. To learn more about making technology work for your organization, connect with us today.

