How single provider experiences give patients better health outcomes
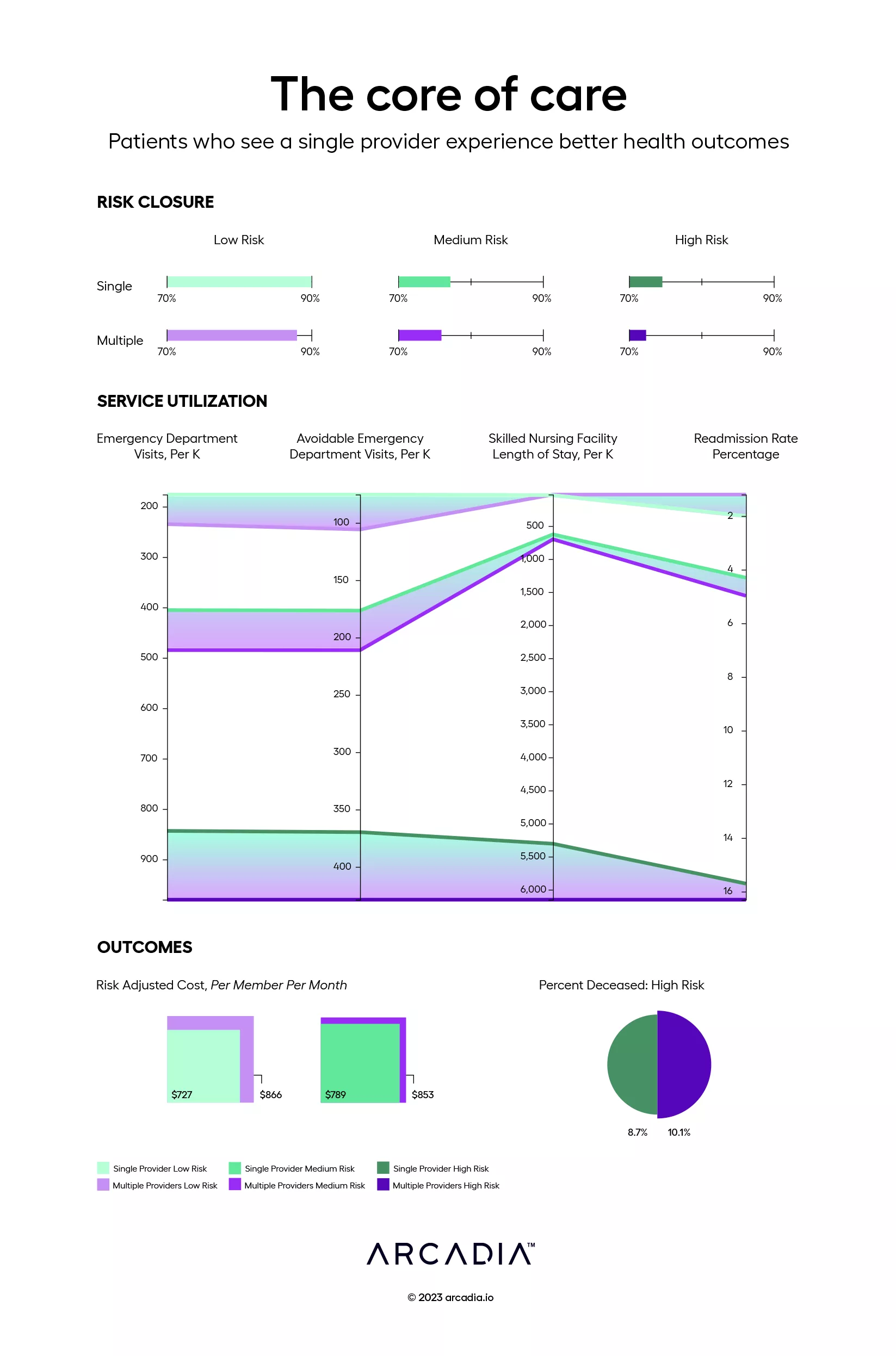
A strong relationship between one patient and one provider leads to better care. It improves utilization, risk closure, mortality, and cost when compared to patients who spread their time between multiple providers. It may seem obvious to say it aloud, but the data backs up what many believe to be true.
The first section in this visualization, “Risk Closure,” shows the percentage closed in low, medium, and high risk patients. The green bars represent patients in Arcadia’s Medicaid population who see a single provider, whereas the purple bars represent patients who spread their time across multiple providers. “Service Utilization,” represents the number of visits (per K) in this same population to the ED and SNFs, along with the percentage of readmissions each risk band experiences. The final section, “Outcomes,” shows risk adjusted cost PMPM in low and medium risk patients alongside mortality rate in high risk patients.
The data is clear: a strong relationship between a single patient and a single provider improves risk closure across the board and leads to better outcomes.
Details
D3.js, Excel, and Illustrator
Data sourced from Arcadia’s Medicare ACO population using claims and clinical surveys
