6 keys that drive success in value-based care
At a glance: Discover how a balanced framework for value-based care — combining strategies to drive revenue with tactics to manage costs — can lead to real success in healthcare. Dr. Luke Hansen shares insights on contract design, network optimization, risk capture, physician performance, optimized utilization, and whole-person care.
Healthcare today often manages to leave patients, providers, and many other stakeholders confused. In our constant pursuit of scientific and technological advancement, improved outcomes and patient experiences, and compounding financial pressures, it often feels like we are being pulled in multiple directions at once. In many ways, value-based care (VBC) points to a solution. By rewarding outcomes rather than volume, VBC aligns incentives around what we truly want as clinicians and leaders: helping people live healthier lives.
Still, achieving success in value-based care comes with its own complexities. At Arcadia, we’ve developed a practical framework that balances two essential facets: driving revenue to fuel growth and high-quality services, while simultaneously managing the costs required to deliver that care. This framework stems from an awareness that a strong strategy must show near-term returns on investment to gain organizational buy-in, while also advancing longer-term transformation by embracing population health and whole-person care.
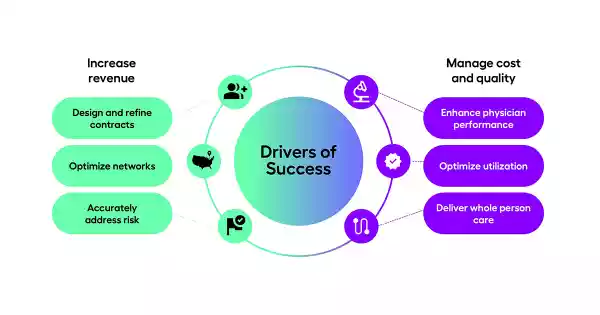
Below, I’ll walk you through six pillars of this framework—three focused on revenue, three on costs—to illustrate how a balanced approach can shape a healthcare organization’s success.
Driving revenue with value-based care: contracts, networks, and accurate risk
1. Design and Refine Contracts
VBC contracts differ significantly from traditional fee-for-service (FFS) agreements. While the FFS model focuses on the volume of procedures and services, value-based contracting incentivizes improved health outcomes.
By intentionally designing contracts that reward real, measurable outcomes, we create a revenue structure that supports the investments we need to make in our organizations. Insight into care and cost variation can inform contracts that drive improvement in high opportunity areas. For example, if you know your network excels at preventive care — like providing timely colorectal cancer screenings — ensure your contracts reflect and reward performance or progress against remaining opportunity. This not only secures revenue but also aligns fee-for-service stakeholders who might still be “in the other canoe,” balancing their focus on procedures with the future of population health.
2. Optimize Networks
The next key element is ensuring that you have the right providers in your network. “Having the right people on the bus” is absolutely critical. Use both your internal (first-party) and publicly available (third-party) data to identify top-performing clinicians and facilities that align with a value-based mindset. An example might be finding orthopedic surgeons who pursue the most rational use of resources — such as outpatient rehab or home-based therapy rather than costly inpatient rehab — when clinically appropriate. Aligning your network around these high-value choices is crucial for generating revenue in a value-based model.
3. Accurately Address Risk
Finally, to receive revenue sufficient to fund necessary clinical services, you must recognize and account for the full clinical complexity of your patient population. Accurate coding of patient conditions — though sometimes seen as a burdensome administrative task—is vital. By ensuring documentation of all appropriate diagnoses, you ensure that your organization receives the appropriate revenue to provide necessary services and can trigger the appropriate next best action for clinical care. Moreover, adopting a broader definition of risk, one that includes socioeconomic and cultural factors, allows you to anticipate barriers to care and deliver more personalized interventions.
Reducing costs sustainably: physician performance, utilization, and whole-person care
1. Enhance Physician Performance
When we look at the cost side of the equation, we often start with physician performance, because it’s so foundational. Historically, physician performance might have focused on select quality measures. Today, it’s about fostering accountability for a fuller range of outcomes — from HEDIS metrics to patient experience and patient-reported outcomes. The goal is not to “teach to the test,” but to truly reduce disease burden through better diagnosis and management. Beyond the HEDIS and other standard measures, advanced analytics that marry signals including EHR data, pharmacy data, and claims data can enable a complex understanding of where quality is delivered as well as where in our complex systems quality fails. For example, robust integrated data can identify not only heart failure outcome variation but also spotlight where in the care process low performing providers are falling short — distinguishing among inadequate access to visits, nonadherence to guideline-directed medical therapy, or failure to confirm medication-taking at home.
2. Optimize Utilization
Optimizing utilization means ensuring that every care decision is aligned with patient needs and resource stewardship. Addressing hospital and ED events that are costly and avoidable including robust risk prediction and real time signaling to enable timely intervention is key to VBC success. This includes matching the right site of service — such as outpatient vs. inpatient — as well as systematically preventing unnecessary low value care. Advancing technology provides us with opportunities to improve access and outcomes while reducing costs without compromising patient outcomes. Every year brings new avenues for procedures and diagnostics to move into more cost-effective settings, so staying agile in how we allocate resources is essential.
3. Deliver Whole-Person Care
Perhaps the most powerful but also the most complex way to control costs is to address patients as whole people — which is to say as they see themselves rather than solely as patients. That means addressing social, cultural, and language needs, helping people overcome barriers like mistrust, inadequate transportation or health literacy, and engaging them in meaningful ways informed by an interoperable data asset. When patients feel known and are cared for in a way that acknowledges their entire life context, we see better engagement, fewer preventable events, and higher satisfaction. Ultimately, that’s better for patients and more sustainable for our healthcare system.
Charting the course to lasting success in value-based care
Succeeding in healthcare today is multifaceted and rightfully daunting. It is critical to address both today’s challenges as well as the strategic opportunities of the future. We’ve seen this six-driver framework facilitate synchronous organizational focus on both tactics and strategy and support near-term wins and long-term value. With organizational focus and discipline informed by robust, data-informed insights we can thrive in a complex and uncertain environment and succeed in value-based care.
The challenges we face in healthcare are considerable, but by continually refining our methods, respecting the complexity of our patient populations, and focusing on quality outcomes, we can ensure that value-based care lives up to its promise: better health for individuals, stronger communities, and a more sustainable future for everyone.
