5 key strategies for ACO performance
There’s no easy formula for success under risk-based contracting, but there are some levers accountable care organizations (ACOs) can pull for better performance in value-based care.
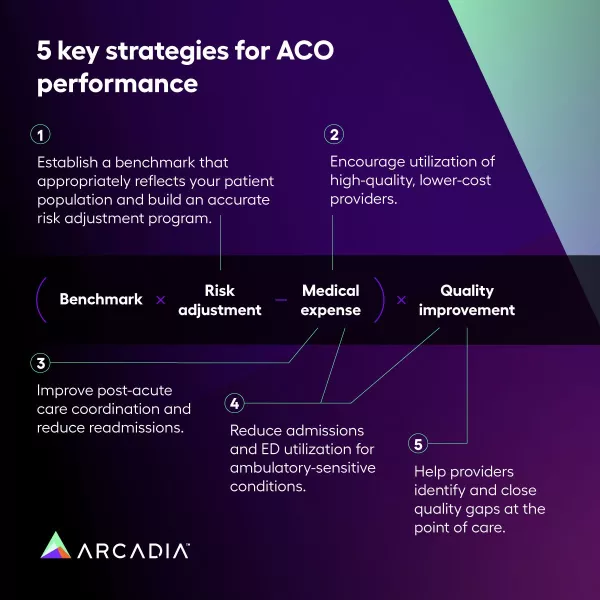
Specific payment models differ between Medicare, Medicaid, and Commercial payers, but ACOs need to develop strategies that address the fundamentals of financial performance in a value-based contract.
Successful ACOs execute against five key strategies.
- Strategy #1: Establish a benchmark that accurately reflects your patient population and build an accurate risk adjustment program
- Strategy #2: Encourage utilization of high-quality, lower-cost providers
- Strategy #3: Improve post-acute care coordination and reduce readmissions
- Strategy #4: Reduce admissions and ED utilization for ambulatory-sensitive conditions
- Strategy #5: Help providers identify and close quality gaps at the point of care
Strategy #1: Build an effective, efficient, and accurate risk adjustment program.
Ensure ACO performance is measured against a benchmark that accurately reflects patient population.
A benchmark is set against which the ACO’s financial performance will be measured. This benchmark is risk-adjusted, meaning that it will be set higher or lower depending on the documented health conditions of the population for which the ACO is assuming risk. The benchmark can be thought of as a global budget under which the ACO must operate.
Depending on the risk-based contract, the benchmark is set in one of two ways:
- The benchmark is set using pre-determined prior year(s) risk adjusted total medical spend or total cost of care. The performance year will be compared to this prior year.
- The benchmark is preliminary, based on prior year(s), with a true up during the performance year.
Build an accurate risk adjustment program.
If the ACO more accurately documents the health concerns of its population, its performance will be evaluated against a more appropriate risk-adjusted benchmark. This can give the ACO a better opportunity to perform well and earn shared savings. Risk adjustment when done accurately will reflect high-risk, high-cost patients preventing a disadvantage for organizations that care for these populations.
The aggregate risk score of a patient is used as a proxy for expected patient cost, and therefore drives provider reimbursement in most value-based payment models. Benchmarks are determined using the aggregate risk score of the population cohort over the course of a 12-month period.
Every year the risk profiles of a patient population reset to zero and must be rebuilt through appropriately documented diagnoses included in the claims data sent to health plans or government payors. High-performing ACOs are constantly focused on ensuring providers are accurately and correctly coding patient conditions and use analytics to identify patients who may have undocumented conditions that required clinical review and intervention.
Strategy #2: Identify high-quality, lower-cost preferred providers.
Reduce total medical expense by improving appropriate care utilization.
During the performance year, the ACO assumes financial responsibility for the care of its patients. If the ACO’s total medical expenses are lower than the predetermined benchmark, the ACO will have the opportunity to share in the savings it generated.
ACOs generally try to reduce total medical expense by improving the appropriate care utilization and care coordination — delivering the right care to the right patient at the right time in the right setting.
Encourage utilization of high-quality, lower-cost preferred providers.
Specialty care and services like MRIs can vary substantially in cost from provider to provider. If patients seek out-of-network care, the ACO incurs higher medical expense and the patients may suffer from poor care coordination.
When an ACO can encourage the use of preferred providers, the ACO can better coordinate patient care across settings while ensuring that the services rendered are of high quality at a lower cost. High-performing ACOs may use technology to make it easier for primary care practice staff to refer patients to preferred providers with availability.
Strategy #3: Improve post-acute care coordination and reduce readmissions.
Post-acute care spend can represent a significant cost for an ACO — with high variability in clinical outcomes across facilities. The most successful ACOs start discharge planning when the patient arrives at the hospital, working with hospitalists and families to match the patient’s clinical needs with the right high-quality, appropriate-cost care setting. These ACOs may partner with narrow networks of post-acute providers like skilled nursing facilities (SNFs) and may establish risk-sharing arrangements that reward positive clinical outcomes, reduced readmissions, and reduced average length of stay.
Strategy #4: Reduce admissions and ED utilization for ambulatory-sensitive conditions.
When patients visit the emergency department or are hospitalized for ambulatory-sensitive conditions, the ACO has missed opportunities to deliver care in a more cost-effective and clinically-appropriate outpatient setting. This drives unnecessary total medical expense for the ACO and can subject patients to experiences that can be painful or scary — with unfamiliar providers.
High-performing ACOs are using tools like predictive algorithms to help their physicians identify patients who are at high risk of inpatient admissions or emergency department utilization and who would benefit from intervention by a care manager. Learn more about using predictive analytics to identify impactable patients for care management.
Strategy #5: Help providers identify and close quality gaps at the point of care.
Improve quality performance to increase access to shared savings.
The goal of these advanced payment models is to incentivize high-value care rather than low-cost care, meaning that ACOs are expected to manage utilization appropriately to deliver good clinical outcomes — cost and quality must be considered in tandem.
ACO clinical outcomes are typically evaluated using a set of quality measures. If the ACO meets or exceeds predetermined quality performance thresholds, the ACO may earn a quality-based bonus, qualify to receive a portion of the savings it generated, or increase the amount of shared savings it earns.
Help providers identify and close quality gaps at the point of care.
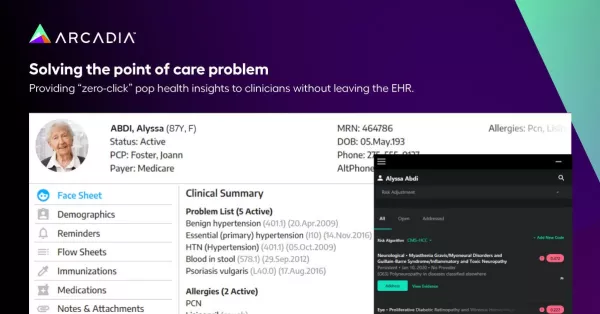
At every encounter, a care team has an opportunity to identify a patient’s unmet clinical needs, deliver the appropriate care, and accurately document the care that was provided. However, poor data and burdensome workflows can be barriers to closing quality gaps.
High-performing ACOs can aggregate clinical information from multiple data sources into an enterprise clinical data lakehouse platform, analyze the data to identify quality gaps, and feed those insights to providers within their existing clinical workflows at the point of care — without making providers leave the EHR or juggle multiple systems.
Building the Successful Accountable Care Organization
With the challenges of increasing cost and quality pressures surpassed only by the uncertainty in the current market, many ACO leaders share concerns about positioning their organizations for success — or even survival. Our ACO Maturity Model provides a framework for assessing your strengths in the seven areas that are critical for success under risk. To learn more, download our white paper 7 Critical Capabilities: Building the Successful Accountable Care Organization.
