An ACO assignment journey: Coding and attribution in medicare ACOs
In this figure, the artists re-imagine the process by which individuals are assigned to an ACO as a battleground, on which ACOs competing for clientele and risk hope to effectively balance their patient load to optimize the utilization of available resources and maximize the creation of shared savings.
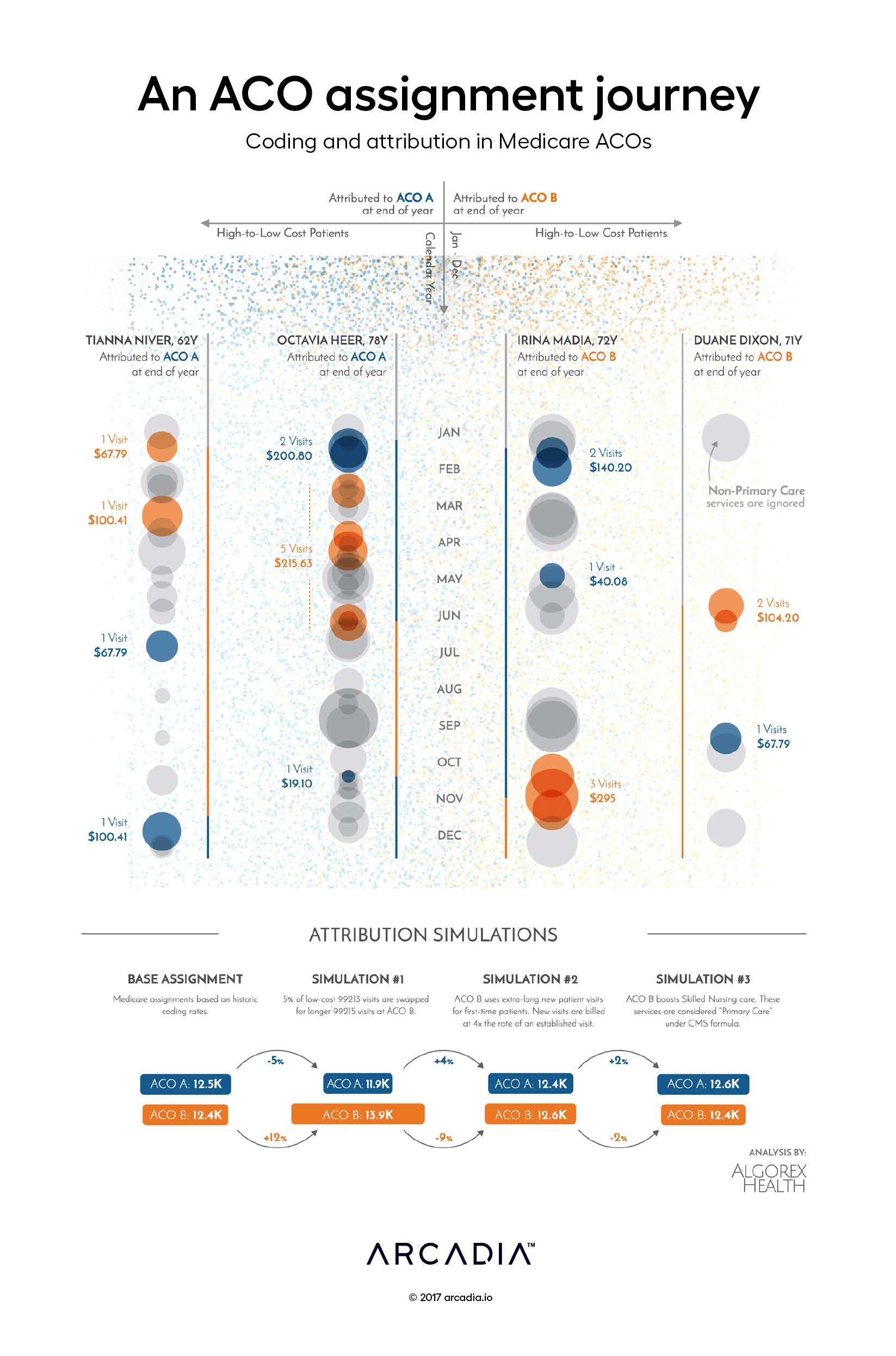
Here, four Medicare beneficiaries are tracked throughout the calendar year. With the behavior (and physician choices) of the beneficiaries fixed — they are unconstrained in the ACO marketplace so this assumption is not too removed from reality — we are forced to consider how the operational choices of the ACO influence the assignment process.
As presented, two of the beneficiaries are assigned to ACO A, while the other two beneficiaries are assigned to ACO B. At the end of the year, this assignment of responsibility will be applied to the ACO, irrespective of their engagement strategy.
However, if we consider the assignment process a strategic effort — a game of optimization — we can explore several opening moves:
First move: ACO B starts an initiative to expand visits by existing patients with certain high-risk conditions, replacing certain moderate acuity visits with detailed evaluations. This results in increased assignments to ACO B, as tie-breaking assignments (like Tianna Niver) side with the costlier provider.
Second move: ACO B expands their new patient visits substantially, billing for those patients at a vastly higher rate. However, this expansion in time results in a drop-in ability to schedule new patients (like Duane Dixon), resulting in lower than expected expansion and a decline in newly assigned members.
Third move: ACO B expands the use of skilled nursing primary care billing. This allows ACO B to count nursing care toward assignments for higher acuity patients (like Octavia Heer), but also replaces some costlier encounters with less expensive nursing encounters, resulting in little net change in assignments.
This battle for assignments continues into the next year, and as the ACOs gather more and better information about their patients, both assigned and unassigned, they continue to strive for the best alignment of their care capabilities, their patients, and their success strategy.
Prepared in collaboration with Algorex Health, helping ACOs use data beyond claims to understand patient engagement.
Details
D3.js SVG, with Illustrator
