Arcadia Customers Outperform National Average in 2024 MSSP
The 2024 results for the Medicare Shared Savings Program (MSSP) mark a milestone in value-based care. According to newly released data from the Centers for Medicare & Medicaid Services (CMS), Accountable Care Organizations (ACOs) delivered the highest shared savings in the program’s 13-year history—evidence of a system that’s evolving toward smarter, more sustainable care.
But not all ACOs performed equally. What set the top performers apart? A clear pattern is emerging. Organizations that harness third-party benchmark data consistently outperform the national average on both shared savings and quality metrics.
In this post, we’ll break down national trends and explore how Arcadia-supported ACOs leveraged third-party performance data to drive better outcomes and higher savings.
Third-Party Benchmark Data Drives Performance
In 2024, Arcadia customers participating in MSSP and leveraging the power of third-party performance benchmark data outperformed the national average in several dimensions.
Earned Savings
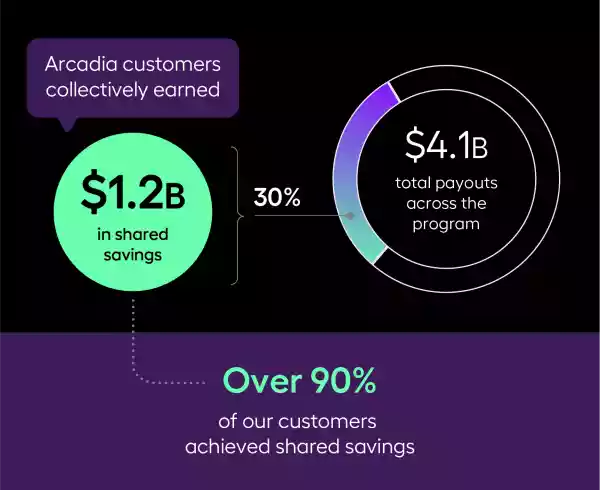
Arcadia customers collectively earned a total of $1.2 billion in shared savings, accounting for nearly 30% of the $4.1 billion total payouts across the program. More than 90% of our customers achieved shared savings, underscoring the strength and consistency of their value-based care strategies, which we enable through our data platform.
Each time an ACO reduces costs, Medicare shares some of those savings with the organization and retains the rest. That retained portion directly benefits the Medicare Trust Fund, making the program more sustainable and easing financial pressure on the healthcare system. This is why value-based models are so critical. They reward providers for delivering better care and remove costs from the system, ensuring Medicare can serve future generations.
Looking more closely at the results, the impact of using Arcadia’s third-party data becomes even clearer. On average, customers leveraging this data achieved $128 more per member per year (PMPY) in earned savings compared to the national average. They also demonstrated stronger year-over-year performance, with an average increased earned savings of $118 PMPY from 2023 to 2024, outpacing the national average increase of $89 PMPY.
Quality Performance
Shared savings tell only part of the story. To fully evaluate performance, quality outcomes must also be considered—and arguably matter even more.
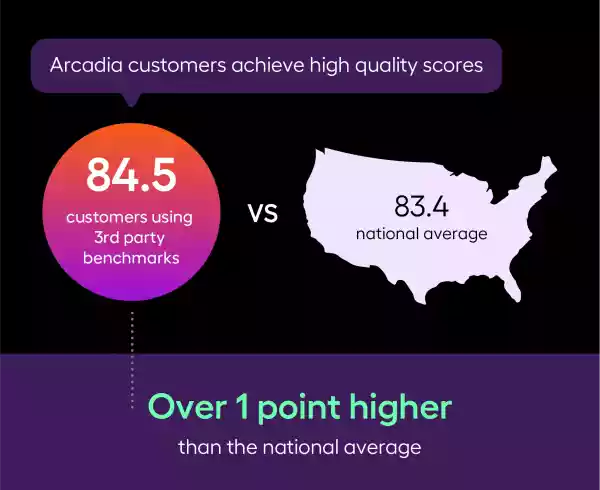
Arcadia customers who leverage third-party benchmarks also deliver stronger quality outcomes. On average, they achieved quality scores of 84.5—more than a whole point higher than the national average of 83.4. This performance advantage underscores how advanced data capabilities can enable organizations to drive financial savings and enhance care quality.
Arcadia customers across the board also excel in keeping patients out of the hospital. As a cohort, Arcadia customers had fewer unplanned admissions among patients with multiple chronic conditions (36.49) compared to the national average (37.03). Inpatient admissions were also lower for Arcadia customers (254.45) compared to the national average (257.83).
Looking beyond the top-line, we see that Arcadia customers using third-party data, on average, performed better in the diabetes control quality measure than the national average. This customer cohort managed to control diabetes for all but roughly 8% of their patients. At the national level, ACOs average 10.5% of their patient population with poorly controlled diabetes.
A percentage point difference may not seem like much on first blush. But let’s dig deeper into the financial implications. In MSSP, one percentage point can mean the difference between receiving the full value of your possible shared savings or a potentially scaled-down rate.
The Value of Third-Party Data

Third-party performance benchmarks are external yardsticks that allow healthcare organizations to measure quality, cost, and outcomes against peers. This is essential for identifying improvement opportunities, negotiating contracts, and ultimately succeeding financially while improving patient care in risk-based contracts.
CareJourney, the company Arcadia acquired in the summer of 2024, is one of the leading producers of third-party performance benchmarks, and ACOs nationwide use them to improve their performance, including in the MSSP. It’s one of the reasons why Arcadia is more deeply integrating CareJourney data and products into our data platform to create a powerful one-stop shop for successful ACOs.
When third-party data coexists with first-party data on the same data platform and workflow tools, organizations can benefit from actionable intelligence to drive targeted performance improvement initiatives and implement near real-time adjustments throughout the plan year.
A Broader Look at ACO Performance
2024 was a successful year for ACOs across the board, not just for those supported by Arcadia. According to CMS, ACOs saved Medicare $2.4 billion in 2024—a new record for MSSP. Net per capita savings increased more than 16% from 2023 to 2024. That number was higher for low-revenue ACOs, which generated $316 in net per capita savings compared to $175 for high-revenue ACOs. This is a trend we’ve seen continue for several years now and is associated with ACOs led by physicians versus hospitals and health systems.
Regardless of high or low revenue, any shared savings earned by an ACO are funds available to reinvest into successful strategies. As pointed out by the National Association of Accountable Care Organizations (NAACOS), prevention and chronic disease management are cornerstones of ACO savings and quality performance. Such strategies helped MSSP ACO achieve lower utilization across various categories in 2024, including hospital admissions, emergency department visits, and length of stay at skilled nursing facilities.
Often, ACOs will fund such efforts to increase access and quality, which further fuel better performance. In 2024, this helped MSSP ACOs impact the health outcomes of patients through better-controlled blood pressure, A1c control, and depression screening when compared to 2023.
Regardless of the type of strategy, they nearly always involve data-driven decision-making, actionable intelligence at the point of care, and robust analytics capabilities that illuminate opportunities in a sea of aggregated data.
Congratulations to all ACOs for their dedication to championing the next chapter of sustainable healthcare.
Editorial Note: CMS notified ACOs that there may be adjustments to 2024 MSSP performance results in the coming weeks. The analysis presented in this article is based on the most recently available version of the published results and is subject to change as updated data is released.
