Building successful risk and quality teams in healthcare: Strategies and best practices
As healthcare evolves and organizations continue to innovate, dedicated risk and quality teams are a critical resource, ensuring patient safety, optimizing care outcomes, and achieving organizational goals. In this article, Arcadia's Maria Mann and Melissa Merenda impactful risk and quality teams. Whether you’re looking to improve an existing team or build one from scratch, read on to learn about how clear objectives, frequent, precise measurements, and customized workflows can set you up for success.
Four steps to build successful risk and quality teams
1. Clearly define goals and objectives: The first crucial step in building a successful risk and quality team is to define clear goals and objectives. By breaking down larger goals into smaller subsets, teams can track their progress over time and celebrate small wins along the way. A well-defined communication strategy is equally important to ensure that all team members are aligned with the set goals and ready to embrace changes.
2. Measure progress: To assess the team's success, it is essential to establish performance metrics early on. These metrics should include program-related data, such as graph capture and recapture rates, provider-related data, and team member productivity. Establishing these metrics allows for continuous improvement and helps the team stay on track to achieve their overall objectives.
3. Identify key focus areas and workflows: Identifying the focus areas of the risk and quality improvement team is crucial for efficient operations. Teams must decide whether they will primarily focus on risk management, quality improvement, or a combination of both. There are a dizzying number of options, Mann says. “What are you going to be working on specifically?” She asks. “Is your team going to do risk? Is your team going to do risk and quality, and what lines of business are you going to cover when you're doing that?” Additionally, the workflows for reviewing patient data can vary, ranging from prospective to concurrent to retrospective reviews. Choosing the appropriate workflow will depend on the team's size and specific goals.
4. Tailor workflows to your team: The size and structure of the risk and quality team can vary across healthcare organizations. Some teams may have dedicated members, while others may embed these roles within different departments. As such, it's essential to tailor workflows to suit the unique needs of your team. You can opt to use specific tools like Arcadia’s Assess for data analysis and reporting, ensuring seamless integration into your existing processes.
Tips for success
To maximize the effectiveness of risk and quality teams, several key tips should be considered:
1. Foster collaboration and communication: Encourage open communication and collaboration between leadership, teams, providers, and support staff. Bi-directional communication enables the exchange of feedback and identification of missed opportunities. “Between the teams, you may have a CDI team, a risk team, and a coding team, so you need those members to communicate,” Mann says.
2. Invest in technology: Efficient technology solutions streamline team processes and improve overall productivity. Investing in advanced tools and systems can help the team stay organized and deliver results more effectively.
3. Leverage data: Utilize data analytics to gain insights into gaps and areas for improvement. Data-driven decision-making empowers the team to identify areas of focus and prioritize actions accordingly.
4. Break up your plan into discrete steps: Create a well-structured plan with smaller milestones to achieve along the way. This approach helps team members feel a sense of progress and success, increasing overall motivation and engagement, and it can help with the adoption of technology. “It’s about small chunks, you know?” Merenda adds. “Metrics to achieve some success, so people feel like they're actually progressing.”
Close the loop and take action
One critical aspect that should not be overlooked is closing the loop. This involves ensuring that recommended actions are followed through and patient care gaps are addressed. Regularly monitoring patient follow-ups and outcomes is essential to the team's success.
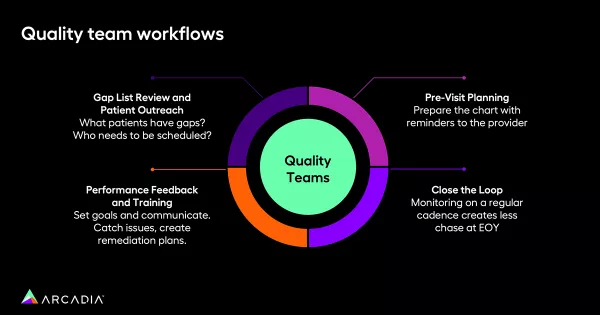
“We're putting those orders in, we're attempting to close those gaps,” Merenda explains. “But it’s also then going back and making sure that you've actually followed up with the patient — that they went and they got the test, and having a workflow to kind of monitor those types of things.”
Powerful teams backed by powerful data
Building successful risk and quality management teams in healthcare requires forethought, intention, and planning. By defining goals, establishing performance metrics, and tailoring workflows to team size and structure, healthcare organizations can maximize the potential of their risk and quality teams.
Collaboration is key. Are you ready to equip your teams with world-class data? See more of our experts discussions on healthcare and data, then reach out to our sales team to learn more.
