In pursuit of health equity: The basics of SDoH for care management
Understanding the intricate factors that contribute to poor health outcomes is essential for delivering effective and equitable care to all individuals. One significant aspect that has garnered increasing attention in recent years is the concept of Social Determinants of Health (SDoH).
These are non-medical factors that influence health, such as socioeconomic status, housing insecurity, and employment instability. Robust data capture at the patient level is crucial for implementing a comprehensive SDoH strategy that addresses these factors.
In this article, we will explore the impact of SDoH on poor health outcomes and the importance of robust data in healthcare decision-making. We addressed this topic in a Byte-Sized Booth Talk at HIMSS, which features Senior Data Analyst, Arjun Gosain. In this discussion, Gosain covers:
- Identifying housing insecurity
- Improvements in member identification
- SDoH concerns and complicated health issues, and
- SDoH observations
The significance of robust data in SDoH strategies
Arjun Gosain, Senior Data Analyst at Arcadia, emphasizes the critical role of robust data capture in implementing effective SDoH strategies. Gosain highlights that a lack of data capture at the patient level hampers healthcare organizations' ability to address SDoH comprehensively.
Gosain states, "A lack of data capture at a patient level is really one of the main reasons why healthcare organizations are not able to implement a robust SDoH strategy."
Gosain goes on to explain that Arcadia conducted pilot analyses to identify the main areas where SDoH data could be captured effectively. For instance, the analysis revealed that housing insecurity is a significant SDoH factor affecting around 65% of populations studied.
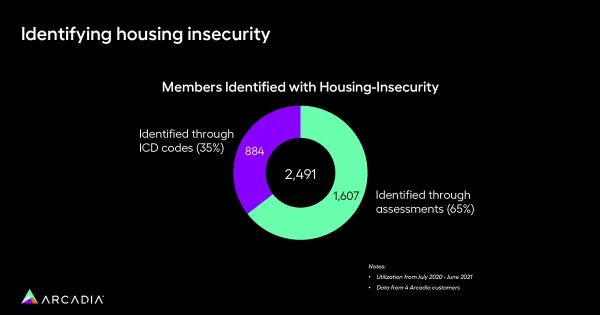
Comparatively, identification through ICD coding and claims accounted for only 35% of patient-level identification. This finding highlights the potential of leveraging assessments beyond traditional coding methods for capturing SDoH information.
Patient identification and impact of SDoH
Through another analysis conducted for a non-profit customer in the Pacific Northwest, Arcadia demonstrated the significant impact of comprehensive patient identification in SDoH strategies. The customer, incentivizing ICD coding, identified an additional 11,000 patients by utilizing a prepared survey integrated into Arcadia's platform.
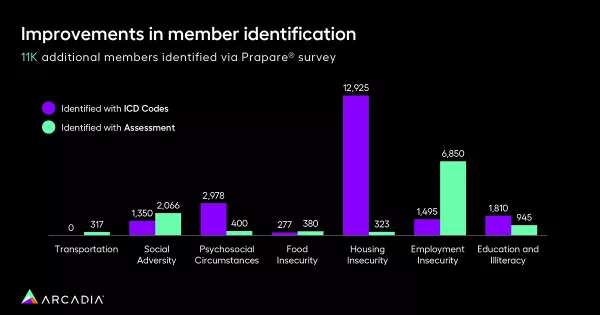
For categories such as employment insecurity, identification through assessments far surpassed identification through ICD codes. This emphasizes the need for diverse data sources to identify SDoH at a patient level.
Creating a robust data set
Arcadia's approach to addressing the data capture challenge involves leveraging a rich data set to develop a robust, clean patient-level registry for SDoH populations. This includes the integration of clinical assessments from electronic health records (EHR) or point-of-care interactions.
Arcadia also offers the flexibility to design customized assessments that align with specific SDoH concepts. ICD codes can be mapped to these concepts, ensuring comprehensive data capture. All these data sources contribute to a unified patient-level registry that feeds into Arcadia's SDoH database and SDoH dashboard.
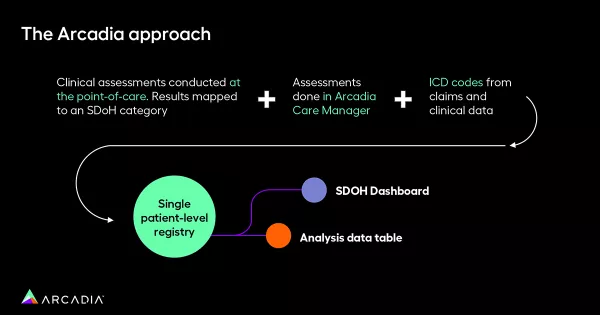
The dashboard allows for in-depth analysis, including geo analysis, outcome monitoring, and demographic mapping on a patient level.
Impact analysis and addressing chronic conditions
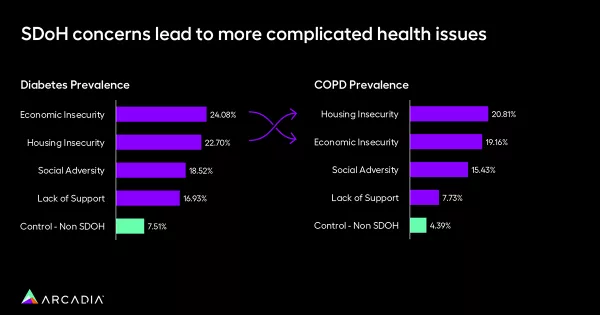
By effectively identifying SDoH at the patient level, healthcare organizations can conduct impact analyses to address prevalent chronic conditions within specific SDoH populations. Gosain emphasizes the importance of such analysis by presenting compelling data.
For example, economically insecure populations have a diabetes prevalence of 24%, significantly higher than the 7.5% prevalence in non-SDoH populations. Similarly, housing insecure populations exhibit a COPD prevalence of 20.8% compared to 4.3% in non-SDoH populations.
These stark differences highlight the urgency of addressing SDoH to tackle chronic conditions effectively.
Financial impact and utilization patterns
Robust data capture on the patient level not only aids in understanding the health impact of SDoH but also provides insights into the financial implications. Arcadia's analysis reveals that members with SDoH are twice as likely to be admitted to the hospital and readmitted within 30 days of discharge. Individuals with housing concerns visit healthcare facilities five times more frequently than those without.
Additionally, SDoH members have six times higher per member per month (PMPM) costs than those without. These findings underscore the need for financial investment in SDoH strategies to alleviate the burden on both patients and healthcare systems.

Key SDoH takeaways
Social Determinants of Health (SDoH) play a significant role in driving poor health outcomes. To address this, healthcare organizations must implement robust data capture strategies at the patient level. Arcadia's approach to SDoH incorporates various data sources, including assessments and ICD coding, to create a comprehensive patient-level registry.
This data enables impactful analysis, highlighting the prevalence of chronic conditions and the financial implications of SDoH. By leveraging robust data, healthcare organizations can develop effective strategies to tackle SDoH and improve health outcomes for all.
Learn more about Arcadia’s health equity applications.
