How to improve your population health using SDoH data
Benefits, challenges, and solutions associated with adding SDoH data to your population health programs
Where a person lives, their access to food, how they were brought up, and even their language fluency factor into their health outcomes. It’s a concept known as social determinants of health (SDoH) and, in fact, the Centers for Medicare and Medicaid Services (CMS.gov) identifies 12 unique categories of SDoH:
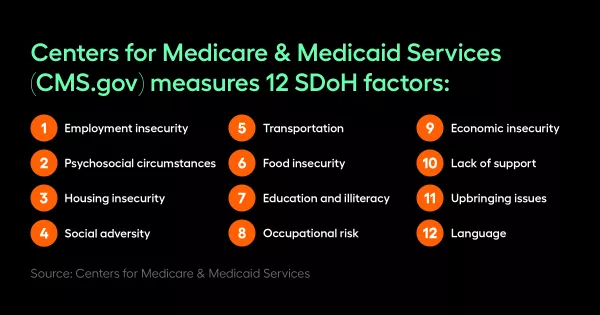
- Employment insecurity
- Psychosocial circumstances
- Housing insecurity
- Social adversity
- Transportation
- Food insecurity
- Education and illeteracy
- Occupational Risk
- Economic insecurity
- Lack of support
- Upbringing issues
- Language
Arjun Gosain, Arcadia Senior Data Analyst, shared that, through an initial proof of concept analysis across different customers, Arcadia confirmed that they do have a really big impact on outcomes.
“We found that members with social concerns are two times more likely to be readmitted within 30 days of discharge. Members with specific housing concerns or homelessness tend to visit the ER five times more than members without that concern. Even members with social adversity have six times higher cost PMPM (per member, per month) annually, when compared to a non-SDOH population,” he described. “When you talk about outcomes, apart from cost and utilization, it also contributes to wide health disparities and inequities. Minority populations tend to be disproportionately affected by them. Therefore, it becomes very imperative to address this issue to help better health outcomes, but also achieve health equity.”
Addressing these factors has become a critical component of healthcare organizations’ efforts to improve patient outcomes.
Jennifer Polello, Community Health Plan of Washington (CHPW) Senior Director of Quality and Population Health, says this process of finding solutions for problems occurring outside of the healthcare setting must be conducted at the individual community-level and can be daunting for organizations to figure out where to start.
She and Gosain spoke with Linnie Green, Arcadia Staff Writer, about identifying and addressing social determinants of health on the Arcadia webinar, SDoH Strategies.
“You may or may not have comprehensive data to show you where you start,” Polello said of the challenge. “We were fortunate enough to look across our population to figure out those areas of greatest needs and where we should focus our resources — employment, housing, food insecurity, and transportation were among our top social needs, and where we decided to build out resources and dig into areas where we could have a greater impact and work with our community partners to understand what challenges lie with within each community.”
SDoH concepts and measures
Two common SDoH are transportation and housing insecurity.
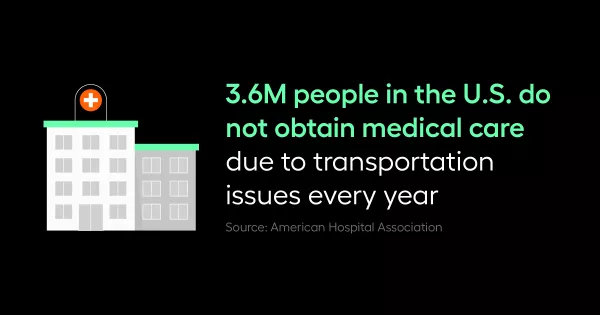
According to the American Hospital Association, 3.6 million people in the United States do not obtain medical care because they do not have transportation. CHPW is attempting to alleviate the negative impact lack of transportation has on its members with a pilot program.
“We're a majority Medicaid plan and reaching those hard-to-reach members is a challenge. We've got an advocate going into members’ homes that are identified as high risk — high risk on the medical side, or social side, or a combination of both,” Polello shared. “These medical advocates visit the members in the home, but often, they're transporting them to a medical appointment and taking them to the pharmacy to make sure that they're getting their medications and helping them figure out their medications in between visits.”
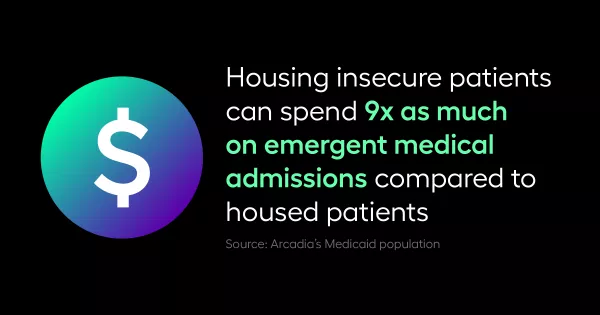
Housing insecurity is another big factor in healthcare outcomes and the cost of care. A study of Arcadia’s Medicaid population revealed that housing insecure patients can spend up to nine times as much on emergent medical care than housed patients.
Solving it requires collaboration with community programs, many of which are overburdened.
“I don't think our state is unique in terms of having way more referrals for housing than there are resources. I think that's a common problem in most communities. And we know that the unhoused have higher medical costs and poor outcomes,” Polello said. “We've partnered with community [organizations] to look at medical respite programs to help members that are discharged from inpatient stay to have some place to rest and recover from their illness. But, we have long wait times for medical respite and general housing resources. I think it looks different across every community, but try to understand what that community landscape looks like and how you can partner with your community organizations.”
Whatever the SDoH factor, the question comes down to who is responsible for finding solutions. Gosain believes everyone should share the burden equally.
“If you ask my opinion, everyone's equally responsible to address such a large issue in healthcare; it cannot be done by one particular stakeholder,” Gosain said. “As Jen said, a strong collaboration between your community resources, your providers, government grants, private companies like ride sharing companies—when they come together and help out each other, we can move a long way in trying to address this issue.”
Three challenges with capturing SDoH data
To address SDoH, organizations first have to understand who the patients are and what they are struggling with. That means capturing the right data that brings critical SDoH information to the forefront to identify the right patients. Unfortunately, there are challenges with capturing SDoH data:
- Lack of ICD codes. “There was always an issue with lack of ICD coding, that there's not enough claims or clinical sources, encounters were getting really coded for those SDoH specific Z-codes,” Gosain said. “I have seen a lot of improvement in the last couple of years, but not up to the mark of really identifying and coding them in a proper good volume.”
- Lack of standardization. “When there's no standard way of collecting data; it makes it very difficult to aggregate all that data and organize and clean that data, to do a robust and really meaningful analysis to predict impacts for these populations,” explained Gosain.
- Using paper surveys to capture the data. Much of the collected data never makes it into the electronic health record (EHR). “We found that a majority [of our CHCs] were using paper surveys, like a prepared template to capture that [data], which is unfortunate because oftentimes that wasn't making it back into the EHR, they had some effort in terms of transferring that data, but that didn't always happen,” Polello said of their review of SDoH data capture across the organization five years ago.
The importance of member engagement
Stigma around SDoH can also make it really difficult for healthcare organizations to capture critical data. They need to give patients the space and privacy to fill out social surveys.
“It's a challenge for providers to ask a patient about their housing status,” Polello noted. “If the provider knows that there's a mile long waitlist for housing resources, they're not going to ask about that, and conversely, if somebody's newly unhoused, being honest to the provider, they may feel their care is impacted if they answer that they're experiencing homelessness.”
Polello recommends turning to stronger partnerships, engaging with a social worker or community health worker that the patient has that social connection with, to assure them that providing this information will enhance their care, not hurt their care.
“Working with our underserved and marginalized communities, often we have undocumented members that are seeking care and they really don't want to share that information and so establishing those personal connections and communications outside of the provider visit has been really helpful in terms of making the patient feel safe and answering and providing that information for us to use across the network,” she added.
Solutions for improving SDoH data capture
After understanding its data capture landscape, CHPWA instituted some changes to its process across the organization that other healthcare organizations could institute as well.
Increase electronic capture of data
“We provided some resources to our CHC's to help them improve their data collection and capture work process and looked at ways to implement an electronic capture of that data, which really helped us improve our ability to see that data,” Polello said.
Implement training with billing teams and encoders on SDoH and Z-codes
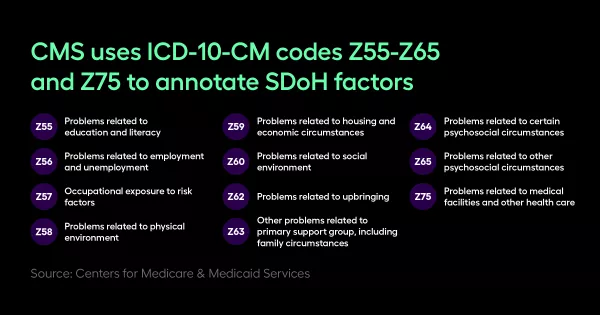
“Help them be more aware of Z-codes and why it's important. It's not always the provider that has to put a Z-code on a claim, for example, and a lot of our CHC's didn't know that a social worker or a biller could add that Z-code to a claim,” Pollelo shared.
Share information from the Plan with CHCs
“We looked at charts or claims that we had received and gave the clinics a list of members that we think were homeless based on the information that we had at the Plan and asked if they could go back and look at those members,” Polello explained. “If they are truly homeless, they add that Z-code and resubmit the claim for us.”
The effort has improved CHPW coding of just on housing alone and the organization plans to branch out to transportation and social isolation as well. Gosain adds proper coding is essential for identifying the right patients.
Technology’s role in putting SDoH data to work for population health
Technology can really go a long way in bridging the gaps that exist.
Gosain says Arcadia uses ICD codes and many other points of data including surveys coming out of point of care EHRs, publicly available sources like census data and the social vulnerability index that CMS provides, and more sources to match with patient level information and identification to get a bigger picture about every patient in the social concern category.
“This information enables us to do more on the predictive analytics side, where instead of prospectively identifying patients, we can actually predict if a patient is likely to have an SDoH concern in the near future,” he said. “Once organizations can define impact, they can justify a proper financial investment into doing a lot more engaging patients and social programs. And also follow up with text message campaigns or surveys to patients to close the loop on identifying patients and connecting them to the different community resources.”
Modern technology tools such as iPads and EHR templates can significantly improve SDoH data capture.
“We've had some CFCs that have started using iPads, for example, with a social assessment on the iPad for members to survey in the waiting room, which has worked really, really well,” said Polello. “We've also worked with some of our providers on incorporating templates into their EHR that is a little bit more standard than capturing some social information in the social tab of their EHR; they've got different templates for different EHRs that are pretty standard.”
Closing the loop for patients
The strategies outlined by Polello and Gosain give healthcare organizations paths forward to improve their SDoH data capture and create appropriate interventions. The importance of data cannot be understated in providing direction.
“Really understanding what your disease burdens are and what your social factors are in your different zip codes that you serve, could really help direct your plan and formulate a really good plan around your first focus because no one can really tackle all social factors right away, even though we would like to,” Gosain said.
He also emphasized that the goal of SDoH strategies is to focus on closing the loop for patients. In the long run it’s important to do the ROI analysis to learn if connecting to a community resource really helps patients and their outcomes.
“Just identifying the right patients and coding and getting the population of different social concerns is not enough,” he said. “When you close that loop of identifying patients and then connecting to resources, you can really do a proper analysis around if a patient identified for housing was connected to a community resource for housing, did that really move the needle on the health outcomes.”
To learn more about how to put your SDoH data to work, explore Arcadia’s SDoH package, or watch the full recording of SDoH Strategies.



