Optimizing care management programs with technology and data analytics
As a National Institutes of Health report points out, the US healthcare system is designed to treat acute medical illnesses, which means patients with chronic conditions or other social determinants of health must regularly navigate a complicated and fragmented system of different providers and conflicting opinions. The report says results of this system include inappropriate, ineffective, or no follow-up care, unnecessary duplication of tests, and inconsistent medication prescriptions with harmful drug interactions.
These results have far-reaching consequences. Managing chronic conditions or handling patients with multiple readmissions has become a costly burden on the entire healthcare system. That’s why finding ways to manage care outside of the hospital setting has grown in recent years. Care management programs have demonstrated that they can be effective at reducing hospital readmission costs, streamlining care delivery, and improving health outcomes, but they can be difficult to manage efficiently.
Connor Navrude, Account Director at Arcadia, Kate Brind, Senior Product Manager at Arcadia, and Lenny Heffernon, Clinical Solutions Engineer at Arcadia discussed the best ways to optimize care management programs and make their management easier for healthcare systems in the webinar, 5 Ways to Optimize Care Management Programs with Technology and Data.
Common programs in care management
Two common care management programs are transitional care management (TCM) and complex care management. Starting the process as soon as possible helps deliver better health outcomes in these instances. For that to happen, Navrude says a care manager needs access to all of the information about that patient's acute visit from various sources at their fingertips.
“Many of our clients use their state RAM health information exchange data to quickly be alerted to any acute visits that come up for a patient in their population in near real time,” he explained. “It allows them to start that TCM process as soon as they're alerted to an acute care visit.”
In addition to identifying TCM patients, care managers must have a longitudinal view of the patient's entire history, which includes historic conditions, if they have a primary care physician that they see frequently, and other data.
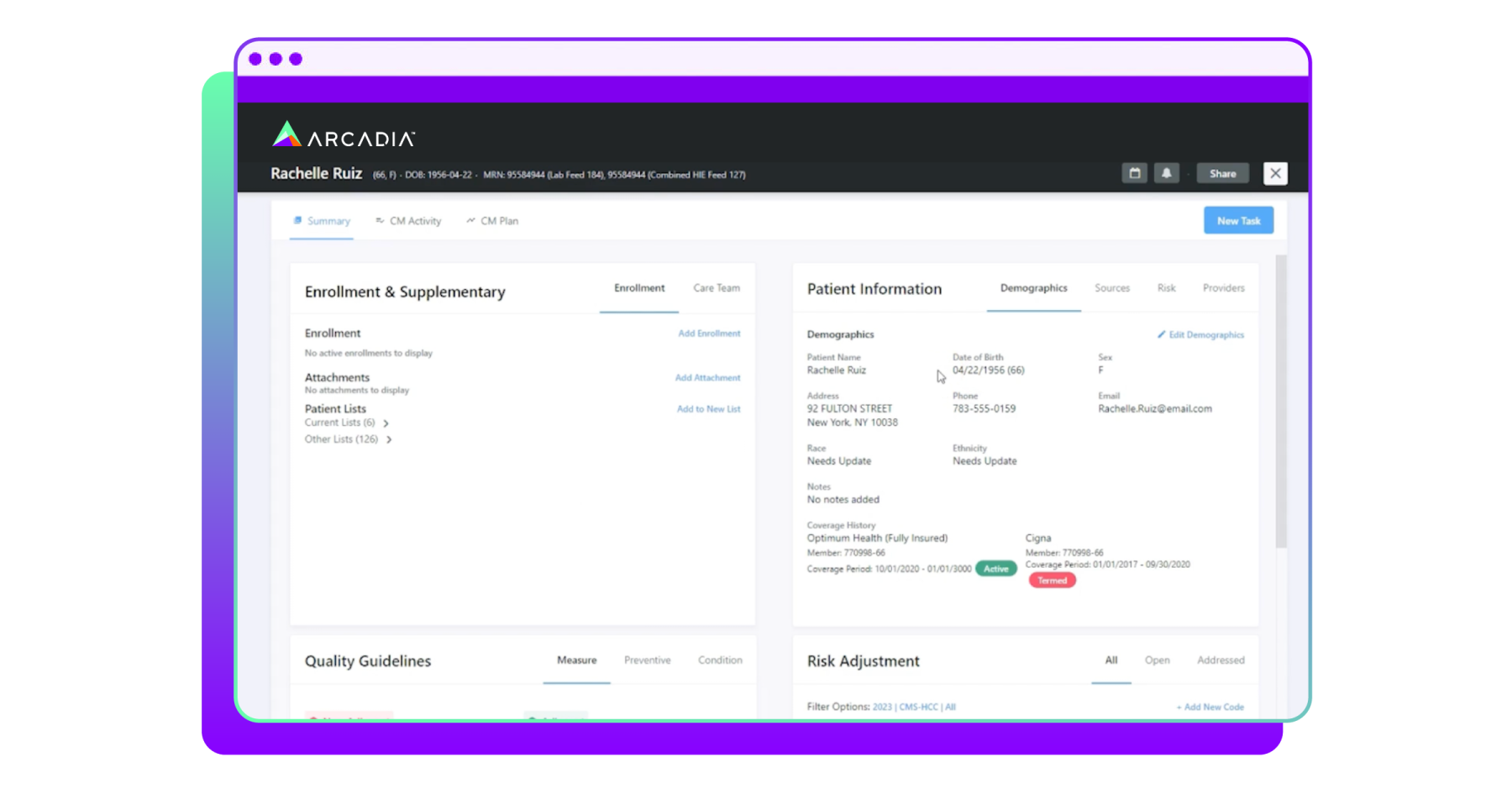
Arcadia gives its clients a 360-degree patient view that shows everything known about the patient based on all the disparate data sources that the health provider brings onto the platform.
“So whether it's coverage history, what's active, what's been termed for that particular patient, we're also going to show you the sources of information,” said Heffernon. “This is how that longitudinal patient record manifests within the Arcadia platform to help those care managers have a complete view of the members that they're engaged with.”
Death by a thousand clicks
For care managers, a lot of frustration and time wasted is the result of clicking through an analytics system to find the one piece of information they need. It has to be easy to navigate through all of the data to get to the point and support the patient. Given their large caseloads, reducing clicks is critical. The platform should front the most appropriate and relevant data so that care managers can take action on actual cases and it should automate redundant tasks.
“There's a lot of opportunity for automation in care management workflows. A lot of what care managers are doing are somewhat repetitive tasks that can be set up and streamlined in a way that every time they go to work with a patient, there are certain steps they should be taking that are the same within each one,” said Brind.
Brind says the automation process takes away the work of the care manager having to schedule, find each assessment, and figure out each day what the patient needs.
“They log in, they see their calendar, and they know what's next for each patient,” she explained. “We can set up care assessments to trigger patients' specific care plan goals and interventions so they know what is relevant to this patient, they don't have to go manually searching for those goals and interventions.”
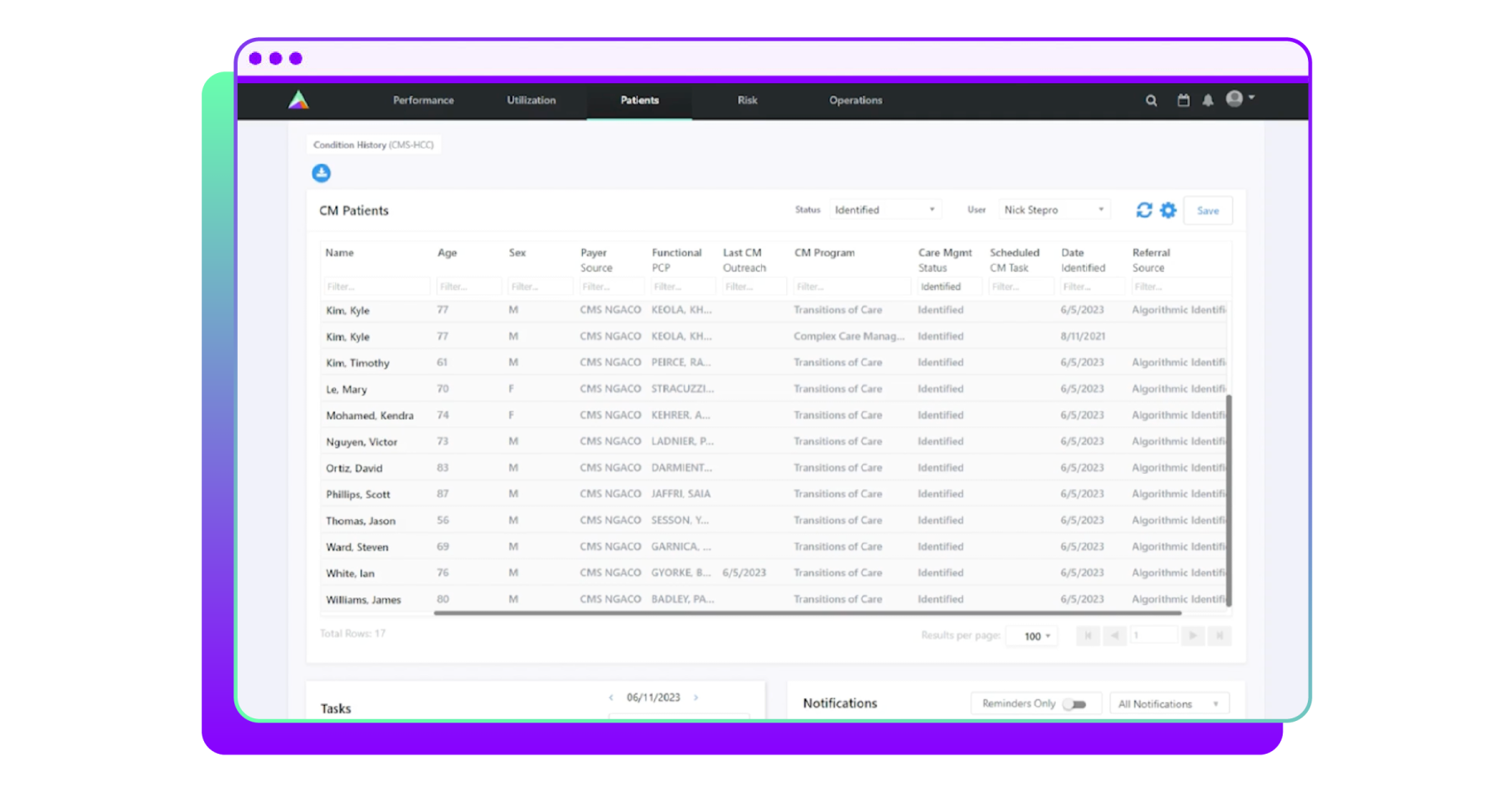
Patient identification automation can use claims data, clinical data, ADT data, and more.
“Whether it's automatically identifying patients for transitions of care management, complex case management, or even identifying those patients who have specific social determinants of health concerns, automating that identification is going to just make sure that the resources are being used at the right time for the right patients,” added Navrude.
Care management cohorts
When it comes to building a cohort of patients, timeliness of generating those cohorts and getting them in front of care managers is critical to success.
“We're not just looking back on data that was generated six months ago; we're looking in real time as ADTs come in for a transitional care program, for example, because we want to get the patient in front of the care manager as fast as possible,” said Brind.
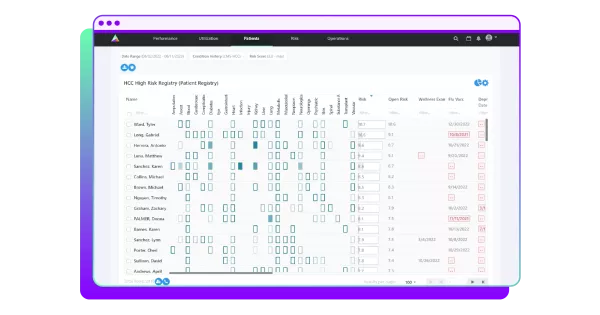
Healthcare systems should also determine which patients will benefit most from a care management program, both in terms of health outcomes and financial impacts. To this end, Arcadia generates an Impactibility Score.
“You can see [from the score] whether there are strong potential, very strong potential, good potential, some potential, or not recommended, and you can prioritize those members that you can have the most impact on, meaning based on a machine learning algorithm built on real world data, these members should have a better outcome, managing their particular conditions at a reduced cost and reducing burden to the healthcare system,” explained Heffernon.
Tracking patient progress
As care management teams prove the efficacy of their work and ensure they are serving patients effectively, they rely on strong reporting metrics.
“Many of these care management teams are really trying to also show, am I reducing costs in my patient population by engaging my MS patients ... so this is really all geared towards ensuring that the investment that our clients are taking in care management services is yielding positive outcomes in the patient population that we're serving with the resources that we have,” said Navrude.
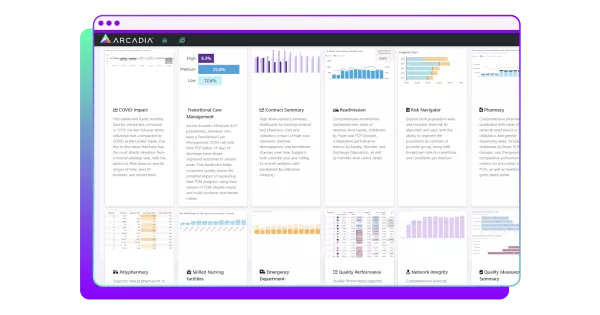
Arcadia’s care management outcomes dashboard shows how a program is performing across a health system's network. It shows metrics that include cost per enrollment, average 30-day readmission rates, and average 30-day emergency department events against the benchmarks.
“It’s real insight into how well your care management teams and programs are affecting your community. So you may want to take these positive outcomes, and start doing some predictive modeling about what would happen if we were to expand our care management programs, or add an additional care manager and focus them on transitional care management,” said Heffernon.
Technology is a key tool for care management success
The common goal healthcare systems work toward is making patients healthier and driving positive outcomes. Making it easy to find the right information quickly, automating tasks, and seeing critical metrics are all necessary for care management programs to thrive and support that goal.
To learn more about ways you can work with Arcadia to implement digital tools effectively for your care management program, watch the full webinar and request a demo.



