Population health management software overview and top picks
Population health management, as defined by the American Hospital Association, is “the process of improving clinical health outcomes of a defined group of individuals.” Success in this wide-reaching approach requires cohesion in every decision that informs healthcare strategies, from illness identification to condition management.
As such, health systems need reliable solutions to organize population data and surface actionable insights that inform decisions. This article answers the most commonly asked questions about population health management software by covering the following topics:
What is population health management software?
Population health management (PHM) software refers to digital tools used to manage the health outcomes of a group of individuals within a predefined population. The goal of PHM software is to provide proactive, value-based care through preventive interventions that reduce the risk of illness progression.
Here is how it works:
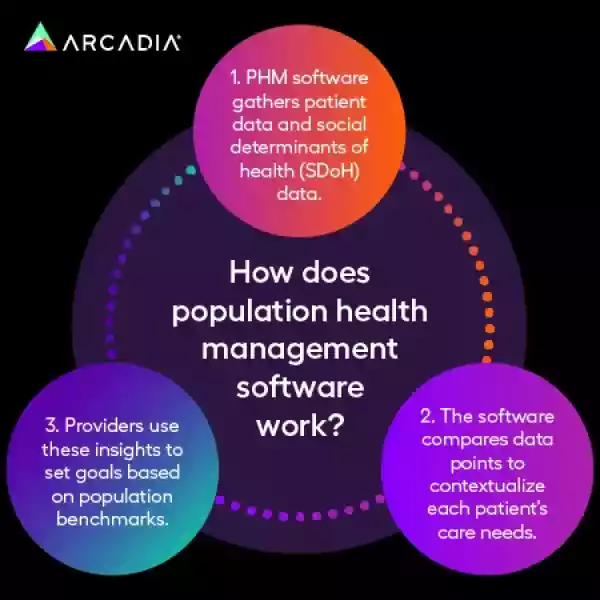
PHM software aggregates data from various sources, including electronic health records (EHRs), self-reported patient data, claims information, and social determinants of health (SDoH).
The software analyzes data points to contextualize each patient’s care needs.
Providers use these insights to set goals based on population and performance benchmarks.
Through this process, population health management solutions enable providers to address preventable health events and better manage costs. This is especially beneficial for addressing chronic conditions, which account for the majority of preventable deaths in the United States and contribute to the nation's $4.9 trillion in annual healthcare costs.
For example, let’s say an organization treats a 61-year-old patient, Jim, who was diagnosed with type 2 diabetes and cardiovascular disease. With PHM software, your organization can match Jim with personalized healthcare recommendations from in-network care teams and programs that will deliver personalized interventions to help manage these two conditions.
What features should health systems look for in population health management software?
Although there are various PHM software providers to choose from, there are a few common features across each solution. These features are built to manage large data volumes so organizations can focus on both large and small populations.
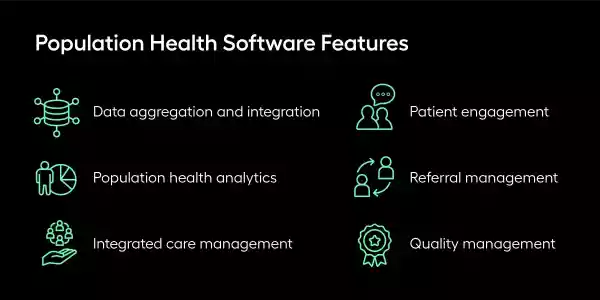
They include:
Data aggregation and integration. PHM software can collect and integrate data from EHRs, insurance claims, patients’ self-reported data, and other sources to offer a comprehensive view of a patient’s health needs.
Population health analytics. With population health analytics, organizations can identify and understand trends and insights related to specific populations, which helps them implement preventive strategies.
Integrated care management. This feature streamlines patient care across various healthcare services, bringing disparate data together under one roof. Integrated care management keeps care consistent and reliable for patients with complex health needs.
Patient engagement. PHM software often includes tools and strategies that enable patients to actively manage their care. These include accessible patient portals, mobile apps, and administrative reminders that promote care plan adherence.
Referral management. When patients need to be referred to specialists or other healthcare services, referral management features streamline the process. This feature also tracks and analyzes referral trends and patterns to maximize positive outcomes.
Quality management. This feature uses performance tracking indicators, health outcomes, and patient satisfaction to monitor and provide suggestions for improving quality performance.
By leveraging all of these features, healthcare organizations can transition from reactive care to proactive health management. However, the specific solution your team chooses will also depend on your population health goals. For instance, you might prioritize finding a solution with user-friendly capabilities that connects disparate care teams. This promotes more effective disease management across different settings and providers.
1. Arcadia
Recognized by KLAS Research as one of the most well-rounded population health management vendors, Arcadia leads the market as a top PHM software provider. Arcadia’s analytics platform offers a solid foundation of data that makes sustainable success possible within a value-based care framework.
Some of Arcadia’s standout features include:
Unified data: Arcadia curates data from clinical EHRs, claims data, social determinants of health (SDoH), pharmacy records, ADT feeds, and other sources, so it’s all visible in one place.
Visual analytics: Intuitive dashboards make it easy to assess population-level trends and insights.
Automated workflow tools: Arcadia’s point of care solutions connect clinicians to data warehouse tables to surface information where decisions and actions occur.
Patient engagement functionality: AI-powered tools streamline patient segmentation and communication, supporting engagement, improved treatment adherence, and overall outcomes.
Performance tracking: Organizations can use real-time analytics dashboards to measure care quality and efficiency and identify opportunities for performance improvement.
Arcadia’s platform enables healthcare systems to drive better outcomes for populations both big and small, complex and textbook. With a solid foundation of unified data, organizations can rely on actionable insights within existing workflows to direct their population health management efforts.
2. CareJourney
CareJourney was acquired by Arcadia in 2024, and together, they equip health organizations with robust provider performance data. Powered by market-leading analytics powered by Medicare, Medicaid, Medicare Advantage, and Commercial claims data, CareJourney enables health teams to improve the effectiveness of efforts to deliver long-term health solutions to whole populations.
3. HealthHelper
HealthHelper is a care coordination tool that specializes in panel management, equipping providers to proactively manage a population’s health needs. This solution’s panel analytics, care gap closure, and detailed reporting tools enable providers to implement targeted interventions that address population health needs before they escalate to adverse health events.
5. J2 Interactive
J2 Interactive’s software development and IT consulting services support health teams navigating complex data and interoperability needs. Especially when tracking patient data and care management efforts across large populations with diverse needs, health teams can deliver improved care at scale with support from J2 Interactive.
6. Castell
While Castell isn’t a dedicated population health management solution, it supports PHM efforts by consolidating and managing payer contracts. Through its partnership with Arcadia, this platform equips providers to streamline value-based contracting so that they can focus more of their efforts on optimizing care for the populations they serve.
7. AthenaHealth
AthenaHealth is a PHM software platform built to help organizations manage multiple EHRs. This solution aggregates, maintains, and normalizes clinical, financial, and payer data to offer organizations reliable data sets. Care teams can quickly assess the right care plans with configurable, evidence-based content.
Then, with help from AthenaHealth, providers can maximize outreach by adjusting their approach to each patient. As healthcare organizations expand, they can rely on reporting dashboards to show cost and utilization across populations.
AthenaHealth also offers a reliable EHR mobile app for patients to log their progress and message care managers on the go.
8. Azara
Azara is a provider of population health solutions for standalone and physician networks, community health centers, and more. Azara engages patients through pre-configured “set it and forget it” programs that automatically initiate patient contact (via text), and track response and follow-up actions.
Additionally, its data analytics capabilities combine EHR data with screening results from SDOH demographic information to create a multi-faceted picture of patient health. Its set of dashboards and reports incorporates data from health plans and other payers with clinical EHR data to offer a detailed utilization view.
9. Conifer Health Solutions
Conifer Health Solutions’ PHM tools are created to prioritize outreach and engagement for people serving hospitals, health systems, and unions.
This solution integrates with health plans to bring pharmacy benefit managers, third-party administrators, provider networks, and other benefit solution vendors together. Specifically, Conifer Health Solutions specializes in personal care nursing, case management, disease management, and utilization management to help members find the right care at the right time.
10. Epic Healthy Planet
With Epic’s PHM suite, Healthy Planet, care teams can monitor patient health and take action with engagement tools. Its data aggregation capabilities eliminate the need for duplicate testing and combine a wide range of data from labs, risk scores, paid claims, and external systems.
The solution provides contract performance and improvement opportunities using analytics to track and intervene on target contact metrics. Epic Healthy Planet also promotes patient wellness with integrated health and social care tools that assess patient needs and connect them with the right resources.
11. i2i Population Health
i2i Population Health technology specializes in providing community health solutions that deliver care for the underserved safety net market. As a healthcare interoperability platform, i2i Population Health leverages scalable data integration services to provide connected services to meet on-demand needs.
The solution’s clinic and in-hospital health application combines workflows with unlimited on-demand registries and reports. Providers also benefit from its standard supplemental data feeds bi-weekly or monthly, with expansive data sets such as SDoH and demographics. Care teams then use insights to enhance coordination and tailor individual care plans.
12. NextGen Population Health Analytics
NextGen Population Health Analytics is a care platform created to offer a clear view of your patient population. This comprehensive software incorporates risk management, cost control, revenue optimization, and targeted interventions.
Specifically, NextGen’s referral management capabilities access information on where patients receive health care services, including specialty care at the population and patient level. It then displays these patient insights alongside patient charts in the EHR.
13. Optum Population Health Solutions
Optum Population Health Solutions is built to help employees choose the right doctor and understand their treatment options and medications. Their main areas of focus are case management, condition management, and cancer support.
The platform’s integrated benefits data enables organizations to analyze performance and financial trends against industry norms and prior performance benchmarks. For example, Optum’s dedicated women’s health programs identify related risk factors and educate mothers and families to reduce complications while lowering costs.
14. Oracle Health
Oracle Health’s technology solutions emphasize chronic condition management and prevention. The platform also has a nationwide network of diverse health systems that conduct clinical trials and outcomes research alongside them.
Oracle Health provides advanced SDoH solutions to intervene at the point of care by using evidence-based screening tools and suggested goals. This way, care teams can keep an eye out for vulnerable populations and make targeted and informed interventions.
15. Clarify Healthcare
Clarify Healthcare’s enterprise analytics platform, Atlas, harnesses the power of big data for business and clinical insights. The platform leverages thousands of trained models to cut and harness data to provide case-mix adjusted predictive values for clear insights.
With Atlas, providers can map the patient journey against predetermined benchmarks and recent trends. This way, they can provide personalized recommendations for each patient based on reliable data.
How does population health management software support value-based care?
PHM software supports value-based care by providing organizations with the tools and insights to balance patient health outcome improvement and cost reduction. Specifically, PHM software enables:
Data-driven care. PHM software allows providers to tailor interventions to individual patients and care plans while monitoring how niche groups compare to broader population trends.
Care coordination. With the right tools, providers can collaborate with stakeholders on every level to assess and track care management notes and patient histories against pre-defined benchmarks.
Risk-sharing models. PHM software uses advanced analytics to categorize patients based on their risk profiles. Providers can use these insights to proactively allocate resources to compensate for higher-risk patients.
Patient engagement. PHM software empowers patients to take control of their health by engaging and communicating efficiently with their care teams. In turn, this engagement can lead to increased care plan adherence and improved outcomes.
Value-based contracting. Through data-driven decision-making, providers can focus on adding quality, efficiency, and overall value to their services rather than the quantity of care. This way, they can reduce unnecessary healthcare utilization.
PHM software aligns all stakeholders — providers, payers, and patients — to drive success in value-based care. When implemented properly, these tools can increase care quality and significantly reduce associated costs.
Final thoughts on population health management software
Modern PHM software reimagines care management with robust analytics and reporting capabilities that allow for coordinated, efficient workflows. As a result, this technology helps reduce overall costs through informed resource allocation that prioritizes high-risk populations.
When deciding which software is right for your organization, choose a solution that will scale with your needs and complement your existing workflows. This will make the transition smoother and provide a higher long-term ROI.














4. Socially Determined
SDoH data holds significant implications for population health, making Socially Determined a critical element of providers’ population health management tech stacks. This platform provides targeted data and analytics for a fuller picture of a patient’s social risk. As a result, health organizations can factor social risks and non-medical health influences into patients’ care plans.