Success in transitional care management (TCM): The first 30 days
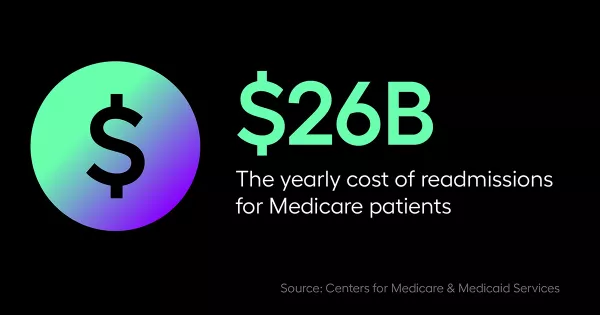
The first 30 days after a patient is discharged from the hospital are the most critical. In fact, The Centers for Medicare and Medicaid Services reports that one-in-five Medicare discharged patients are readmitted within this time period. This costs $26 billion per year for Medicare patients.
In Arcadia’s Byte-Sized Insights, Michele Winiarz, System Director, Quality and Patient Safety Population Health at Ascension Illinois / AMITA Health ACO / CIN spoke with Andrea Purjue, Director, Enterprise Partnerships at Arcadia about the reductions in readmissions her organization saw when patients saw their provider within 30 days of discharge and how they worked to improve their transitional care management (TCM) program.
Hone in on primary care providers
Transitional care management services occur during the period between inpatient care and a community setting. Often, TCM services are handled by primary care providers. When Ascension Illinois / AMITA Health ACO / CIN decided to develop the skills set to dig into the claims data to see who wasn’t already being served by the care management team, they realized they needed to drill down to the provider level to make change in the ambulatory space.
“We found that from a quality perspective, we can hone in on those primary care providers to see how can we help them, what data did they need, how could we help drive the initiative to try to get more patients in to see them after discharge?” said Winiarz.
Best practices for overcoming barriers to TCM
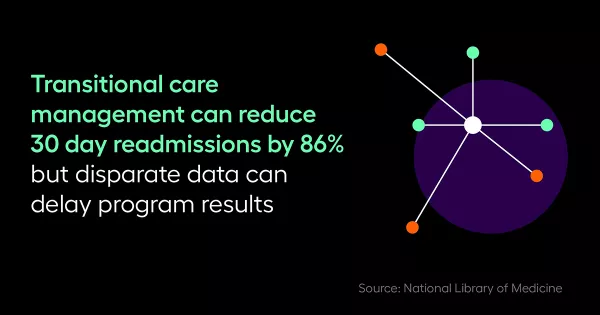
Even though Ascension Illinois / AMITA Health ACO / CIN knew how they could improve their TCM program, two big barriers stood in their way. Winiarz says they had to find ways to get their providers' access to data in a timely manner and share the data securely.
“We have so many independent providers, we have a lot of EHRs,” said Winiarz. “Many of them are small, independent practices so they don’t have integrated systems with the hospitals so they don’t get discharge information in a timely manner — that by far was the biggest barrier.”
To solve this challenge, Ascension Illinois / AMITA Health ACO / CIN received access to the Arcadia population health platform, which allowed the providers to see the patients in the same way the care management team does.
The value of integrated technical resources
TCM can create value across multiple payment models. Specifically, Ascension Illinois / AMITA Health ACO / CIN has found that adding this level of technical resources adds value in three important components of care. First, it helps cost benchmarks and keep costs lower. Second, it helps providers within their network grow volumes by giving them the opportunity to re-engage with patients who may have been lost to follow-up care in the past. And third, it helps the organization re-establish its network by bringing patients back in who have gone elsewhere because they didn’t know they should have followed up with their doctor.
“This is exactly what is needed,” said Purjue.
Transitional care management improves quality
“All roads lead to quality,” said Winiarz.
TCM has been shown to improve quality. Primary care providers are the gatekeepers who keep everything in check after discharge, reducing readmissions and maintaining patient safety.
Watch more Byte-Sized Insights or request a demo to see how we can put your data to work, together.
