Care management software: Key features and top providers
Teams across the care continuum must provide effective, whole-person care at controlled costs to best serve patient populations and ensure organizational efficiency. However, with moving parts like complex patient needs, disparate patient data, and data tracking barriers, it can be easy for your organization to get out of rhythm, resulting in misaligned resources and prematurely cut programs.
This is where care management software comes into play. By facilitating everything from patient identification to care plan formulation to case management, these tools improve coordination and data transparency to support cost-effective health management.
In this guide, we’ll cover the basics of care management software, including:
- What is care management software?
- Benefits of care management software
- 7 top care management software platform providers
- How to choose a care management platform
These tools have widespread benefits. As you read through this guide, note that real examples of health teams using this software are an excellent source of information about its wide range of use cases.
What is care management software?
Care management software includes the tools and technologies your organization uses to manage and coordinate patient care. The goal of care management is to facilitate informed and proactive intervention strategies that improve the quality of care.
Specifically, care management software streamlines the various aspects of patient management, including:
- Treatment planning
- Medication management
- Healthcare service coordination
It provides a reliable source of updated measurement information that reduces the risk of misaligned resources and unreliable results.
With help from a robust care management platform, healthcare organizations can count on comprehensive, data-backed support for every patient’s journey, from program identification to results interpretation.
What are the features of a robust care management platform?
Care management platforms provide a simple way for care managers to access an overview of every aspect of care delivery. A robust software solution uses the following features to support increased data aggregation and interoperability:
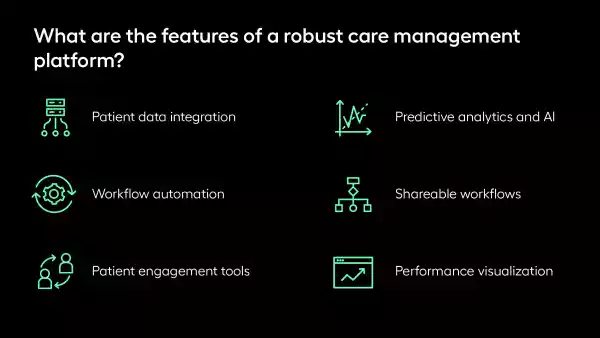
- Patient data integration consolidates medical records, history, and treatment plans into one accessible platform, eliminating data silos.
- Workflow automation streamlines burdensome administrative tasks and clinical processes to keep managers informed and up to date.
- Patient engagement tools facilitate and support ongoing patient-provider interaction, from initial outreach to end-program assessment.
- Predictive analytics and AI analyze historical data to anticipate and prevent negative health outcomes using machine learning.
- Shareable workflows coordinate care between teams, enabling organizations to collaborate with confidence.
- Performance visualization tracks and displays provider performance to aid in clinical improvement efforts.
Care management software saves time and reduces costs with the above features. With continued use, your team can refine its operational efficiency and focus on caring for your patients instead of chasing data points.
Benefits of care management software
A robust care management platform can benefit various teams. Let’s look at some of the benefits realized from leveraging this software.
Supports the patient journey
The best way to assess healthcare technology is to examine its features at work. Care management software provides a comprehensive framework to support patients throughout their experience, from initial assessment to ongoing care and outcome evaluation. For example, let’s explore how the right platform supports three pivotal care management objectives:
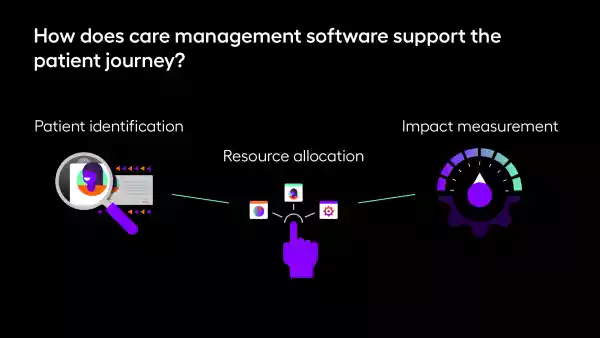
- Patient identification: Care management platforms enable teams to dig deep into patient histories to identify and analyze eligible populations. Then, members can use specialized tools to pinpoint risk factors and create actionable prevention plans.
- Resource allocation: Proactively allocate staff and resources by using the platform to match potential cases to the right managers. Then, leverage predictive analytics to prioritize at-risk populations and customize outreach.
- Impact measurement: Keep a pulse on your performance with platform case control and retrospective review. As a team, you can then communicate your findings to key stakeholders, schedule automated assessments, and course correct over time.
Effective care requires precise decision-making. A robust care management platform can help you future-proof your operations, maximize resources, and administer informed care plans.
Enhances care coordination
Payers have a significant impact on member access to care management programs. A reliable provider network is the key to effective care coordination, meaning payers must establish a network of quality providers and incentivize members to leverage appropriate resources. This involves offering financial incentives, employing effective outreach, and even covering care coordination services.
Care management software plays a critical role in this process by:
- Improving resource allocation: Analytics tools enable payers to identify high-risk patients, prioritize interventions, and allocate resources accordingly
- Enhancing data integration: Care management software makes patient information accessible to the teams that need it, fostering collaboration between payers and providers
- Reducing healthcare costs: The emergence of AI and predictive modeling helps payers identify preventable health events, like hospital readmissions, and helps providers intervene proactively
- Automating workflows: From patient outreach to decision-making, care management platforms reduce administrative burden by automating communication tasks
As a result, these capabilities support not only payers’ workflows but also the member experience.
7 top care management software platform providers
Let’s explore seven platforms that can revolutionize your workflows. Browse our list of top providers or watch the video summary below.
Arcadia
Arcadia’s library of care management applications enables care teams to tackle transitional care management, chronic care management, and nonclinical care coordination with confidence. Here’s an overview of our platform's robust, configurable, and automated workflows:
Arcadia’s care management module:
- Equips team members to surface risk factors that guide nuanced, specific programs
- Applies predictive models to patient data so team members can estimate costs and allocate resources efficiently
- Stratifies impacted populations for tailored outreach
- Measures impact at automated intervals
Arcadia enables you to align your team and access the information you need at the point of care. Our robust data set and predictive analytics are there to help guide your team through every step of the care journey, supporting informed and productive action all while recouping time and maximizing resources.

Athenahealth
Athenahealth is a cloud-based healthcare management service, including EHR integration, revenue cycle management, and population health tools. The platform’s standout features include patient engagement tools, advisory services, care coordination, and telehealth support.
In addition, AthenaPatient mobile services increase care access so patients can log their progress and message care managers on the go.

AssureCare
AssureCare serves payers, providers, pharmacies, and the government to enhance transitional care management, reduce treatment delays, and coordinate with pharmacists. The platform combines utilization management, care management, and medication therapy management for a threefold solution for synchronized care.
AssureCare is known for care coordination, care planning, risk assessment, population health analytics, and tools for patient engagement to support value-based care.

HealthEdge
Health Edge’s care management solution, GuidingCare, is a comprehensive platform for whole-person care that simplifies workflows for both health plans and providers. Its next-generation data integration and workflow management tools facilitate coordination and collaboration, accelerate quality improvement, and promote provider and patient engagement.
GuidingCare specializes in health plan administration and core administrative processing for payers with automated care planning, community referrals, and mobile clinician access.

ShiftCare
ShiftCare zeroes in on home and community-based care management solutions, helping organizations coordinate care to clients in non-institutional settings. The platform’s progress tracking and sharing, accessible care plans, family access, goal tracking, and document management system help care teams meet their goals and establish good relationships.
ShiftCare also includes a mobile app and a dedicated family portal, so all parties can stay informed on the latest care developments.

Helios Care Management
Helios Care Management provides broad spectrum visibility to promote care coordination, collaboration, and value-based care delivery. It is available in different product tiers and configuration levels based on your team’s management needs. With user-friendly point-and-click tools, the platform facilitates more efficient day-to-day use.
Helios’ commitment to security also underpins its software as it has been HITRUST-certified across care, disease, utilization, and population health management tools.

Cognizant Health
Cognizant Health seeks to integrate as many care management processes as possible through its shared CareAdvance and Value-Based Benefits solutions which are both hosted on a member portal. In turn, this automates providers’ authorization and utilization management processes to help lower costs and improve care quality.
Cognizant Health uses touchless operation processing to automate prior authorization processes for providers to get more immediate approvals that meet business requirements and clinical guidelines.
How to choose a care management platform
As you search for the right care management software that fits your needs, there may be several questions you’re juggling — the most prominent one is probably, “How do I know which platform is best for me?” To guide your decision-making, your chosen solution should:

- Provide high ROI and is within your budget
- Be user-friendly and complement your existing workflows
- Have reliable security and customer support
- Have a reputation for high patient engagement
- Be customizable and will scale with your processes over time
- Facilitate seamless care coordination
Consider these must-haves and add any additional deal breakers to your decision-making criteria. For example, if an organization specializes in chronic disease management, it needs a solution that tracks and visualizes long-term patient data effectively.
Care management: Conclusion and additional resources
The goal of care management is to match patients with early intervention strategies that improve the quality of care. Care management software supports this effort by providing tools for patient data analysis and management, facilitating personalized care plans, enabling efficient coordination among providers, and offering platforms for patient engagement.
