Strategies for successful Transitional Care Management programs
A 7-step process for improving your ACO’s MSSP results
Arcadia’s ACO customers enrolled in the Medicare Shared Savings Program (MSSP) had another record year, generating $10.7 million of average savings per customer, and once again outperforming market benchmarks.
So what sets these ACOs apart?
We’ve identified three areas of opportunity for ACOs that have helped our customers succeed in a changing marketplace:
- Transitional Care Management (TCM)
- End of Life Care
- Percentage of Members with Annual Wellness Visits (AWV’s)
This article will dive into the first area, Transitional Care Management (TCM). After reading, you’ll walk away with some valuable strategies to improve the results of your organization’s programs.
What is Transitional Care Management (TCM)?
When a patient is discharged after an inpatient stay, there’s a concept of managing the patient’s transition out of the hospital. That’s TCM.
This is typically a 30 day management cycle. The primary goal is to ensure that the patient doesn’t need to be readmitted to the hospital unnecessarily.
ACOs new to value-based care may ask, “Should I implement a program like this?” while those who already practice TCM are likely thinking, “How do I optimize my program?”
What is the best way to run a TCM program?
There are many different ways to run a TCM program, but Arcadia customers performing well in this area typically follow this core approach:
- Identify members discharged from hospitals through ADT data
- Help PCPs schedule TCM visits with their patients
- Track TCM visit performance at the PCP level
Wherever this approach exists, providers inevitably see reduced medical expenses, reduced readmissions, and a shift in care from the inpatient setting to the outpatient office visit setting.
This is great because those outpatient office visits mean more revenue for providers and a reduction in spend from the value-based care perspective.
What are the primary challenges in running a successful TCM program?
Jacob Hochberg, Arcadia’s Executive Director of Customer Insights, says he sees four main areas where ACOs can improve performance and achieve similar results to Arcadia’s MSSP customers.
Challenge #1: Patient outreach
There is a real incentive for PCPs to bill TCM codes because they get paid an extra $100 when they do.
The challenge? These PCPs have to meet certain criteria to qualify. Primarily they have to outreach to the patient within two days of discharge, then see the patient within 7 or 14 days depending on the code they use.
ACOs who supplement this outreach criteria and empower their PCPs with tools to make it easy, perform better.
Challenge #2: Individualized care plans
PCPs also have to develop a care plan for each patient to receive TCM incentives.
That means extra time developing the plan, but also walking the patient through it and making sure everyone is on the same page. That’s a big pressure for providers used to billing fee-for-service.
Challenge #3: PCP adoption
This area is a symptom of the first two. PCPs may see the extra work it takes to bill TCM codes as a burden and decide not to engage in the practice.
The shift to value-based care, Hochberg says, requires ACOs to support PCPs in shifting their thinking. This extra time spent reaching out to patients and developing care plans means savings down the line and better outcomes for patients. It also means increased revenue under value-based care models since providers share in savings.
Challenge #4: Good data hygiene
For ACOs to properly support their PCPs in these activities, they need to know when patients are discharged so they can monitor how many enter into TCM programs and the rate of success for those that receive an individualized care plan.
Hochberg says that requires good data hygiene, which can be challenging for certain groups.
ACOs, however, who invest in the infrastructure to identify these data points, develop a process, and promote this to their PCPs find better results. These results, as evidenced by Arcadia’s MSSP customers, are a great way to justify investment and properly measure outcomes.
How can ACOs encourage their PCPs to adopt TCM?
That probably leaves you with the question of how ACOs can encourage their PCPs to adopt these practices.
Based on what he’s seeing work with Arcadia customers, Hochberg described a 7-step process for ACOs to follow:
- Identify Discharged Patients
- Prioritize Highest Risk Patients
- Make Outreach Easy
- Support Care Management
- Measure Outcomes
- Support Struggling PCPs
- Share Metrics with Providers
Let’s explore what this looks like in practice:
1. Identify discharged patients
Arcadia’s ACO clients with exceptional MSSP results use Admission, Discharge, Transfer (ADT) data integrated with their Population Health Software to identify which patients have been discharged. They can see who has been assigned a TCM code and who hasn’t.
2. Prioritize highest risk patients
ACOs also marry these ADT data to claims and clinical data to identify their highest risk patients who have recently been discharged. This is where analytics becomes insight.
Identifying high risk patients is crucial in prioritizing where to focus to improve overall outcomes, and predictive modeling can help stratify patients with high or rising risk.
3. Make outreach easy
Patient outreach is among the greatest challenges in implementing a successful TCM program. Arcadia’s ACO clients have solved the problem by automating outreach for PCPs.
To get an idea of how ACOs can make outreach easy for PCPs, take a look at this case study. It covers how a large pediatric CIN identified high risk populations who deferred well-child visits during the COVID-19 pandemic. Once they identified these patients, the CIN sent notifications to educate parents and caregivers and support their primary care practices. This resulted in a 47% increase in patient encounters for participating PCPs.
4. Support care management activities
Outreach is one thing. Ensuring patients aren’t slipping through the cracks is another.
High performing ACOs invest in care management programs, and equip care teams with the tools needed to effectively manage patient care, target and close care gaps, and track and perform patient outreach.
5. Measure outcomes
They also measure and report outcomes on a regular basis. Typically, this should be reported at the provider level so operational leaders can identify high and low volume providers.
6. Support struggling PCPs
An example of decision-making aided by these reports is an ACO deciding which PCPs to give greater support. High performing ACOs can gain insight into who is following through with TCM visits, identify PCPs who are lagging behind, and deliver specialized attention to improve results.
7. Share metrics with providers
ACOs that performed well in Arcadia’s MSSP results also make it a habit to push metrics out to their providers. They regularly share reports with doctors that reinforce the principles behind value-based care.
Hochberg says these reports convey to doctors that, “Hey, we’re going to bonus you based on how well you perform in this key metric. And we’re also going to give you the ability to keep track of where you are and how you stack up against other physicians.”
This is the number one thing in Hochberg’s view that ACOs have to drive success in value-based care is physician incentive models.
All of this leads to better outcomes — for everyone.
So to recap, Transitional Care Management visits are defined as the % of discharges from an acute inpatient event with a TCM code typically billed within 14 days of discharge.
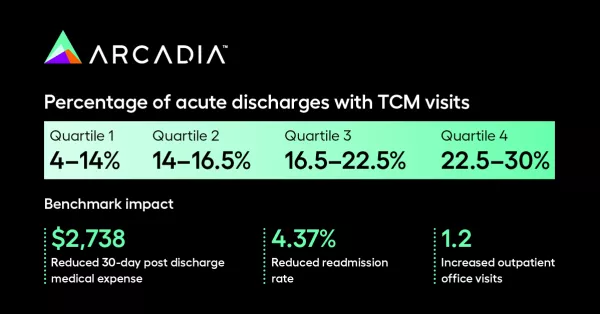
Arcadia’s ACO customers have consistently outperformed the market as evidenced by the latest MSSP results report. This means:
- Reduced costs
- Reduced readmissions
- Increased outpatient office visits
These outcomes improve financial and operational results for both ACOs and PCPs. Patients and populations also see an improvement in overall care.
What about the other two areas for improving MSSP results?
At the beginning of this article, we listed three areas of opportunity for ACOs that have helped our customers outperform MSSP benchmarks:
- Transitional Care Management (TCM)
- End of Life Care
- Percentage of Members with Annual Wellness Visits (AWV’s)
If you’re interested in learning what ACOs are doing to perform well in each area, sign up to get notified when these articles are published. In the meantime, download the 7 Critical Capabilities of an ACO white paper, or book a consultation with an Arcadia expert.
