The power of healthcare data analytics in end-of-life care programs
Hospice is a sensitive topic, and data analytics can help organizations improve performance and honor patients’ agency
Here, we’ll explore the relationship between healthcare data analytics and end-of-life care programs with Dr. Rich Parker and Arcadia VP of Analytics and Chief Analytics Officer Jake Hochberg, highlighting how data can illuminate potential benefits and opportunities for end-of-life programs to improve. With insights from professionals in the field, we shed light on the importance of data-driven decision-making and its impact on delivering excellent care during this critical stage of life.
Understanding patient preferences and achieving dignified care
Dr. Parker, who has years of experience and continues to work in hospice care, emphasizes that it’s important to address patients’ wishes during their final days. Most patients express a desire to be at home, surrounded by loved ones, to be comfortable, and to be treated with dignity. By equipping doctors and the healthcare system with the necessary tools and data, it becomes possible to fulfill these desires effectively, in part or in whole.
“If you ask a patient or a family member, ‘What would your wishes be,’ usually — almost always — people say, ‘I’d like to die at home with my family present, and I’d like to be comfortable. I’d like to have some dignity,’” Dr. Parker explains. “And the good news is, that’s all achievable if doctors and the systems that support doctors have the tools that we need to get that work done.”
Combining data with physician expertise
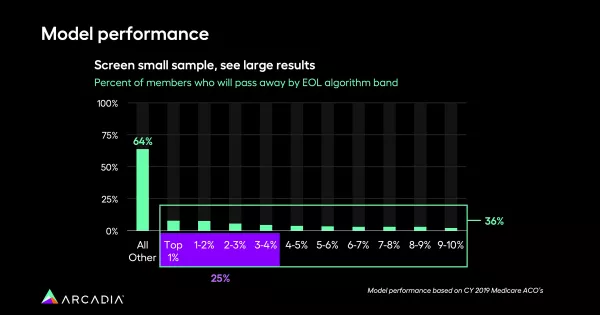
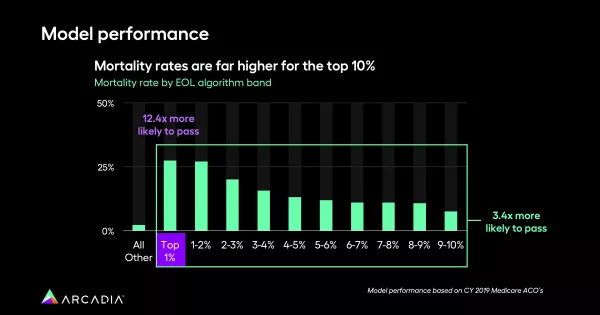
The most successful end-of-life and hospice care programs combine a data-driven approach with empathy. Healthcare data analytics are similarly collaborative. By combining the Arcadia algorithms with a physician’s clinical expertise, providers can identify patients who are eligible for hospice care. By leveraging data insights, healthcare professionals can zero in on patients who frequently visit, display signs of severe illness, and have multiple comorbidities, ultimately leading to more effective care provision.
Doctors with an average panel of 2,000 patients can’t sift through information at the speed of an algorithm, so analytics are a tool they can wield for accuracy.
“If you say to that doctor, ‘Tell me who are your patients who you think are eligible for hospice in the next six months, or the next 12 months, you’re going to get a blank stare, because our brains don’t work that way,” Dr. Parker says.
“But on the other hand, if you take the Arcadia algorithms, you run their data, you give them a list of, say, 100 patients, then you can say: ‘Now of these 100 patients, which do you think will be eligible for hospice in the next six to 12 months?’ They’re going to know, because these are the patients that come in frequently, they’re sick, they have multiple comorbidities. And so, by combining the Arcadia algorithm with the doctor’s brain, you’re going to end up with the right list of patients to put more effort into.”

The financial implications of good hospice care
While humane, high-quality care is the ultimate goal of a hospice program, it’s worth noting that these offerings can ultimately save healthcare organizations money, a double benefit that makes providing great care more sustainable.
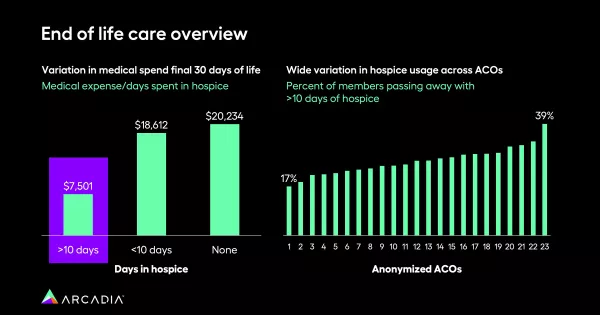
Dr. Parker points out that when patients receive more than 10 days of hospice care, the costs associated with end-of-life care are relatively low. However, if patients receive less than 10 days of hospice care or no hospice care at all, costs spike significantly, reaching up to $18,000.
Leveraging data for improved end-of-life care
By incorporating data analytics into their end-of-life programs, healthcare providers can identify areas for improvement, set benchmarks, and measure their performance. With access to robust, contextualized data that’s constantly updated, providers can assess where they stand in terms of patients receiving adequate hospice care.
Data analytics can be a window into the length of patients’ stay in a hospice environment.
“Across our customer base, there’s a wide spread in terms of how many patients are passing away with 10 plus days of hospice,” Hochberg says.
At some facilities, only 17% of patients die after 10+ days in a program, whereas on the higher end, 39% of patients are dying after these longer stays. The highest percentage of enrollees are in hospice during their final one or two days of life, and critically, these numbers reflect people who are already in the ICU — meaning this data will help hospitals make better decisions around resource allocation, and potentially have better discernment around the best candidates for admission.
Additionally, Hochberg explains, data analytics can flag which doctors are referring the most patients, or underutilizing services.
Empathetic, impactful healthcare at every stage of life
The marriage of healthcare data analytics and end-of-life care programs holds great potential for improving patient outcomes and optimizing resource allocation. By leveraging data insights and predictive analytics, providers can align care delivery with patient preferences, ensure dignified and comfortable end-of-life experiences, and achieve cost savings in the process. Healthcare organizations can flag patients nearing the end of their life to involve them in decision making, respecting their agency, and crafting an informed end-of-life plan.
Want to ensure happier, healthier days for all, from birth to death? We can help with that. Learn more about how Arcadia’s data analytics platform works, and how it can help you unblock better performance.
