Optimize employee health management with data analytics
Keeping a large employee population healthy and engaged is a formidable task, comprised of many moving parts. But it’s not impossible — data analytics is a powerful ally.
Herding cats. Balancing spinning plates. Playing whac-a-mole. Whatever metaphor resonates, the idea of keeping a large employee population healthy and engaged in their care is a formidable task, comprised of many moving parts. But it’s not impossible to optimize and streamline group health plans — data analytics is a powerful ally, as Director of Enterprise Partnerships recently Joe Graffy explained.
Patient stratification in group health plans
In a recent session, Graffy delved into the challenges faced and solutions implemented by a large health system with around 100,000 employees across the United States, primarily concentrated in the Midwest. In this instance, the system used a third-party administrator (TPA) to pay their claims and extend their network nationally. This set-up allowed the organization (and others like it) to extend benefits across geographical borders, which is especially critical for remote employees.
“The goal is to equitably incentivize all of your beneficiaries to engage in healthier behaviors throughout the year,” Graffy explained. “So what this customer did is they broke their population into two general buckets, and then one of those they further subdivided.”
This includes a “bucket” for young and healthy employee health plan enrollees, then another for chronic conditions like diabetes or hypertension. The latter group was further subdivided into high and low-risk individuals, to impart a sense of who would benefit most from care management programs.
One of the primary challenges in employee healthcare management is ensuring equitable benefits for all employees, regardless of their health conditions. Striking a balance between incentivizing healthier behaviors and managing chronic conditions — providing an equitable experience for everyone on staff, regardless of their current state — can be daunting.
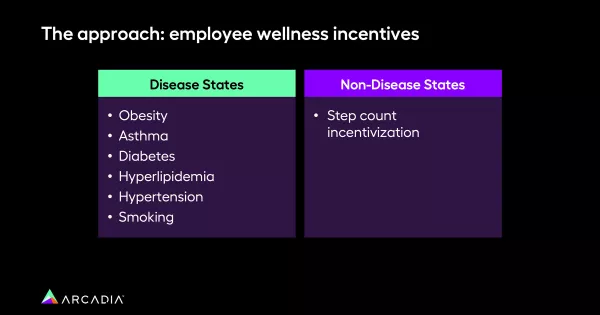
For non-disease states, employees were encouraged to maintain an active lifestyle. Those who reached their step-count goals over the year received premium reductions. Meanwhile, employees with chronic conditions were enrolled in care management programs, with different levels of incentives based on their risk profile. This approach ensured equitable benefits while promoting health-conscious choices.
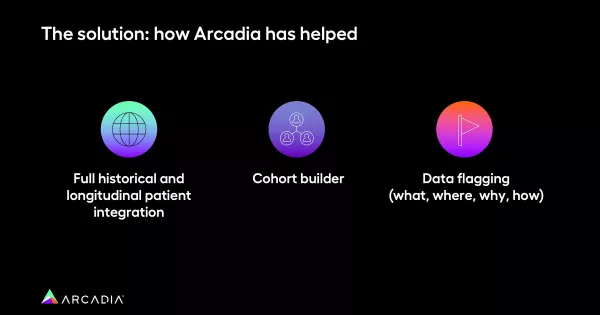
The crucial aspect of this process was data analytics. Graffy emphasized the importance of leveraging data to refine the cohorts of disease states effectively. With inexpertly applied or imperfect algorithms, there’s a large instance of false positives — pregnant women being flagged for obesity, for example — and reducing these errors subsequently reduces the workload of care managers.

Data quality: A critical challenge
Data quality was another significant concern for the employee health plan. With over 200 data feeds and disparate electronic health records (EHRs), ensuring synchronized and accurate data was a daunting task. The asynchronicity of data across sources made it impossible to track individuals' health trends throughout the year, leading to inefficiencies and individuals "gaming" the system.
Arcadia's solution involved integrating historical data from multiple sources into a single, longitudinal patient record within our SQL database. This allowed for comprehensive tracking of individuals' health journeys, enabling a better understanding of why they were flagged for enrollment in specific programs. Care managers could then make informed decisions about appeals, reducing the time spent on false positives.
“Something you hear in the healthcare space that has merit everywhere is: you can’t manage what you don’t track,” Graffy said. “You can’t manage what you don’t measure.”
Aiming for continuous improvement, one data point at a time
As the health system enters the first year of evaluation, the focus is on continuous improvement. By analyzing the performance of different cohorts, understanding cost structures, and identifying effective care pathways, they aim to further refine their approach and automate processes. The overarching goal is to create a streamlined, data-driven system that optimizes employee healthcare management while reducing the burden on care managers.
“Now that we have these cohorts flagged, our question will be: how do these cohorts perform?” Graffy added. “How much do these cohorts cost to manage? What care pathways are effective for managing the cost for the for these cohorts? And then, once you understand those triggers: how can you make those systems more automated and efficient?”
Your partner in health plan performance
Managing the health of an employee population is a complex endeavor, but data analytics provides a powerful tool to navigate the challenges. By categorizing employees into appropriate cohorts, incentivizing healthier behaviors, and fine-tuning the algorithms used, organizations can strike the delicate balance between equitable benefits and efficient healthcare management. The journey towards optimizing employee health is an ongoing one, but luckily, data analytics lead the way.
Interested in leveraging analytic insights to drive a healthier employee population? Arcadia can help.
Click below to watch Graffy’s entire talk, then reach out to a member of our sales team to learn how data can enable your company’s vision.
