How to use healthcare payer analytics for financial success
In healthcare, payer analytics offer crucial insights for reducing costs and increasing revenue. However, a survey conducted by Arcadia and Healthcare Dive found that, despite payers reporting they’ve maintained comprehensive health records for members, many struggle to fully maximize the analytical power of their datasets. Specifically:
41% of survey participants reported difficulty deriving insights from their data.
39% found it difficult to aggregate clinical and claims data.
37% faced challenges enabling providers with shared workflow tooling.
35% struggled to operationalize or act on data insights.
A successful analytics strategy hinges on a few key factors — namely, the technology that payers employ. This article explores how payers can fully harness their data through tech-driven analytics.
FAQs about payer analytics
What is healthcare payer analytics?
Healthcare payer analytics is the process of combining payer data with structured data from provider networks and analyzing it to improve performance. This process relies on technology such as automation, real-time data, artificial intelligence (AI), machine learning (ML), and predictive analytics.
Ultimately, the insights derived from healthcare payer analytics drive economic success under Medicare, Medicaid, and commercial risk-based contracts.
What are the different types of payer analytics?
Payers can formulate health plans, adjust services, assess risks, and control costs by leveraging insights gained from various analytics methodologies. These methodologies, or types, of data analytics for payers include:

Provider analytics
This type of payer analytics leverages provider performance data to evaluate the effectiveness of practices within the network. Relevant data could include:
Cost efficiency
Resource utilization
Adherence to evidence-based clinical guidelines
Clinical outcomes
Provider performance data offers key insights into care quality and efficiency. By using a dedicated analytics solution, payers can monitor provider performance and compare it to industry benchmarks to identify opportunities for improvement. Ultimately, applying these data-driven insights leads to demonstrable improvements in the quality, efficiency, and value of care delivered across the entire network.
Population health analytics
Population health analytics surfaces health trends and disparities by analyzing data such as:
Lab results
Pharmacy records
Social determinants of health (SDoH) data
Electronic health records (EHRs)
These insights guide more targeted interventions, enabling providers to prevent avoidable health events and manage costs more efficiently.
Predictive analytics
Predictive analytics applies algorithms to historical and current data to make predictions about future events. For payers, this type of analytics forecasts:
Future care needs
Preventable care utilization
Members’ potential costs
Incidents of potential fraud, waste, and abuse
The ultimate goal of predictive analytics is to enable a prescriptive strategy for payers to mitigate unnecessary costs and allocate resources more efficiently.
Claims analytics
Claims data offers insight into health demands and necessary resources, helping payers allocate health services where they’re most needed. Relevant data may include:
Care utilization, including which services members are accessing, frequency of use, and potential gaps or overutilization in care pathways
Costs of care for different populations, procedures, and providers
Care effectiveness based on the outcomes resulting from specific interventions
Analytics tools enable payers to look beyond historical claims data and forecast future health needs. This way, payers can proactively mitigate escalating costs more effectively.
Risk adjustment analytics
Risk adjustment data offers insight into healthcare payments, enabling payers to establish more accurate financial arrangements based on health risk profiles. This type of payer analytics is critical for accurate patient stratification, which categorizes members according to their:
Demographic information
Specific risks
Disease profiles
Risk adjustment analytics supports a financially stable and fair healthcare system where reimbursement accurately reflects the cost of caring for individuals with diverse and complex health needs.
Reporting analytics
Healthcare payer analytics plays a vital role in fostering collaboration and alignment across the entire healthcare ecosystem. Reporting analytics enables payers to collaborate with a diverse range of other teams, including providers, care managers, and executive leadership.
The method of collaboration involves:
Interactive reports
Data visualizations
With reporting analytics tools, payers can leverage filtered views to access actionable insights into their data. This ensures that complex information is distilled into clear takeaways that drive collaborative decision-making aimed at improving overall system efficiency.
How do healthcare analytics benefit payers?
After applying a strong data analytics framework to their workflows, payers can experience numerous benefits. Here are just a few of the possibilities:
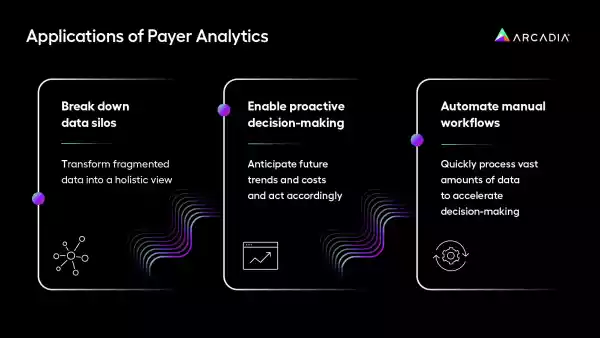
Break down data silos
Healthcare payer analytics solutions transform fragmented data into a holistic view of clinical, financial, and operational information. With a unified view of each member, payers can drive improvements in care management for both cost and care quality for enhancements.
Enable proactive decision-making
Advanced analytics breaks down barriers to collaboration across teams. Access to real-time insights paired with the power of predictive analytics empowers payers to make decisions at the point of care, anticipate future trends and costs, and act accordingly.
Automate manual workflows
From claims processing to care management to utilization review, healthcare payer analytics solutions eliminate time-consuming workflows. With automation tools, payers can quickly process vast amounts of data to accelerate decision-making. Not to mention, automated workflows reduce the risk of manual errors and strengthen data privacy measures.
Challenges addressed by healthcare payer analytics
With the right technical solution, payers can address several challenges through analytics. For example, consider how Arcadia’s healthcare payer analytics solution addresses the following common challenges:
1. Challenge: Developing and managing a high-performing network
A network of high-performing providers is critical to quality care and cost efficiency. Payers often find building and retaining this network challenging, especially in such a highly competitive market. Analytics enables payers to achieve this network by ranking providers, modeling network configurations, and optimizing payment structures. As a result, payers incentivize high-quality and cost-effective care.
Solution: Use a healthcare payer analytics solution to identify top-performing providers, model effective networks, and strategize compensation.
2. Challenge: Optimizing risk management and documentation
Payers must assess patient risk for accurate premiums, reimbursement rates, and risk adjustments. However, data fragmentation makes capturing risk data difficult. Healthcare payer analytics enables payers to collaborate seamlessly with providers to understand relevant care factors and accurately assign risk scores.
Solution: Identify opportunities to capture risk and streamline coder and auditor workflows through payer data analytics.
3. Challenge: Controlling the cost of health services and pharmaceuticals
Healthcare costs continue to rise, making it increasingly important for payers to manage the cost and accessibility of care. Analytics supports this in several ways:
- Identifying high-cost prescriptions, which allows payers to negotiate prices and highlight cost-effective alternatives
- Benchmarking care utilization to identify outliers and areas for improvement
- Analyzing episodes of care, such as surgeries or chronic disease management, to compare costs and outcomes
Solution: Apply analytics to monitor costs, utilization, and outcomes to identify cost drivers and intervene accordingly.
How to build a healthcare payer analytics strategy
While the right technology streamlines data aggregation and analysis, payers must have a well-developed strategy in place to put healthcare payer analytics to work. Follow these steps to do so:
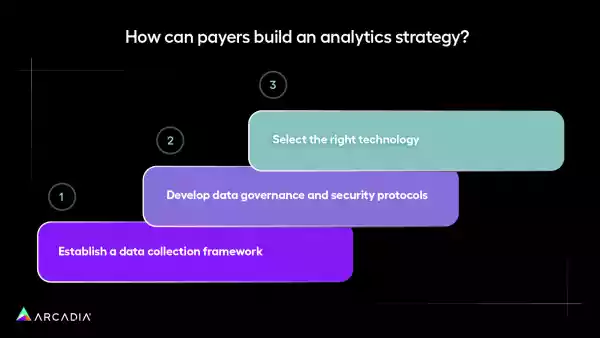
1. Establish a data collection framework
Start by creating a strong foundation for data collection by ensuring that all data is accounted for and consolidated. Don’t leave out any data sources, including:
- Claims data
- Electronic health records (EHRs)
- Pharmacy records
- Provider performance metrics
Prioritize systems that support real-time data collection and create a plan for integrating data from diverse sources. Additionally, check for interoperability between systems to ensure seamless data flow.
2. Develop data governance and security protocols
The healthcare sector has seen an increasing number of data breaches over the past decade, becoming one of the top industries threatened by data breaches. To be exact, healthcare organizations saw 491 data breaches in 2024, resulting in over 58,668,002 breached files.
To enhance security, payers must prioritize data privacy. This involves creating standards for:
- Data ownership and access: Implement role-based access controls to limit data exposure. Establish robust security measures, including data encryption and regular audits, to prevent breaches.
- Data quality: Identify reliable data sources and outline data governance policies to ensure your data provides accurate insights. Assign individuals to oversee data quality and ensure compliance with relevant regulations.
- Data security training: Mandate security training for all team members handling patient data. This training equips payers to identify potential threats, such as phishing emails, and respond appropriately, reducing the risk of human errors.
Additionally, payers must foster a data-driven culture to promote collaboration and ensure a seamless analytics process.
3. Select the right technology
Healthcare payer analytics solutions serve a critical role in extracting insights from relevant data.
Ultimately, your healthcare payer analytics solution should help you achieve four key drivers of success:
- Best managing a population
- Meaningfully decreasing costs
- Increasing revenue
- Expanding member footprint
Selecting the right solution, like Arcadia’s data platform, equips payers with technology capable of collecting, consolidating, and storing data in real-time — then turning large volumes of data into actionable insights. Additionally, healthcare payer analytics solutions enable payers to reduce administrative burdens while continuing to deliver highly personalized reports to providers and employer groups.
Partner with a data analytics company today
Healthcare payer analytics is a transformative tool for payers. With effective planning, continuous improvement, and the right technology, payers can unlock insights that drive cost efficiency and high-quality care.
An experienced and reputable analytics company will supply the reports, tools, and support your organization needs to extract meaningful insights. Explore Arcadia’s payer analytics solution to discover how you can harness the power of your data to create best-in-class health experiences.
