From risky business to sustainable financial performance in value-based care
The first step in lowering risk, maximizing reimbursements, and succeeding in value-based care is building a solid population health strategy. Learn how data analytics helps healthcare organizations refine their approach to population health and use limited resources for maximum impact.
If the impact of healthcare is measured life by life, improvement by improvement, how can healthcare organizations scale these ambitions for large, complex populations? It’s a question that’s top of mind for everyone from individual hospitals to CMS, which recently announced its goal to have every member on a value-based care plan by 2030 as part of the Making Care Primary initiative.
Here, learn how recent CMS data reveals winning strategies of top performing healthcare organizations, and how you can emulate that strategy with a focus on primary care, care management, and data analytics. From one patient to an entire population, better outcomes start with actionable information.
Primary care: the home base of the healthcare journey
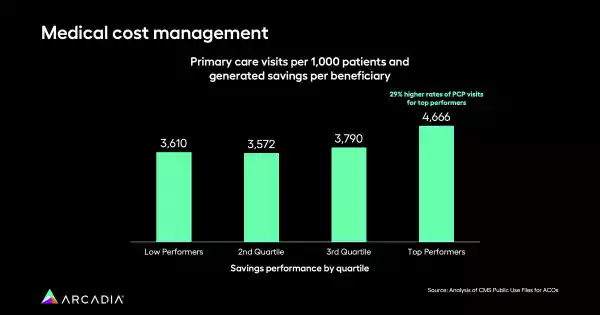
Primary care is instrumental in driving better outcomes in value-based care. It’s the first stop on a patient’s journey, and it can be their introduction into a larger healthcare system. A primary care physician is often a patient’s main healthcare contact, and the first line of defense if something goes wrong. Analysis of publicly reported CMS data over three years shows that organizations with the highest rates of primary care visits were also the best fiscal performers. The top quartile had a 29% higher rate of PCP visits compared to their lower-performing counterparts.
Consistent primary care also engages patients. It helps them feel connected to a particular healthcare system, driving adherence, and with consistent primary care visits, providers and care managers have a timely sense of how a patient’s doing (and what additional services, if any, they might need).
These findings prove just how critical primary care is to larger population health strategies. For organizations to thrive, investing in essential population health competencies is critical. This includes ensuring access to care, maintaining network integrity, and providing sufficient resources and providers to facilitate timely patient access. It also means investing in care teams and management, striving for excellent clinical documentation, and employing care coordinators and community health workers for social determinants of health screenings.
In a recent discussion between Dr. Kate Behan, Chief Medical Officer at Arcadia, and Michele Winiarz, PA-C, Director, Provider Performance & Quality Improvement at AMITA Health, Winiarz emphasized the necessity of continuing these investments despite the rising cost of labor and a primary care shortage.
“It’s really important that organizations understand that they can’t take their foot off the accelerator when it comes to these types of programs,” she says.
Tackle chronic disease to improve overall outcomes
Chronic diseases are some of the most difficult to treat, but they’re also some of the most important — and potentially costly. Managing diseases like hypertension at the population level is another key component of excellent VBC performance, and preventive care can save healthcare systems untold amounts that would otherwise be spent on admissions or in emergency departments.
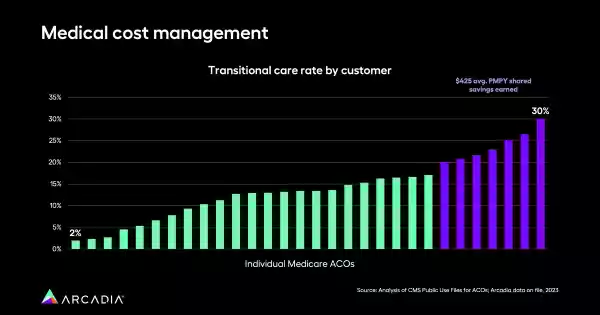
The most successful organizations in the CMS dataset prioritized these concerns, illustrating the power of an interconnected system that includes primary care, care management, and transitional care programs. Regular visits allow providers and care managers to keep abreast of the patient's condition and determine if additional services are required, and these frequent check-ins give healthcare systems a steady stream of data to better understand a patient’s changing health.
Transitional care ensures that a patient doesn’t fall off the map, and helps to make sure that they’re following the care plan that’s most likely to succeed. This proactive approach prevents larger, costlier, and more time-consuming issues down the line, and offers patients a consistent touchpoint with their care team.
Data analytics’ role in advancing better population health
Merely executing care management, transitional care, or primary care programs isn’t enough — data and analytics are indispensable for evaluating their success. These are the tools that let healthcare organizations monitor what’s working and what isn’t, then refine their approaches for the highest impact.
Patient segmentation is one major feature of a data platform that powers excellent programs. Using a data platform, care managers and administrators can segment patient populations for targeted care management, focusing on individuals with specific disease profiles or risk factors. This precision saves time, so users spend fewer hours manually sifting through files. Additionally, it lets program administrators see who’s most likely to be impacted by an intervention, so they can allot resources where they’ll go furthest.
From a healthy population to healthy reimbursements
Through strategic investments in primary care, chronic disease management, and data analytics, healthcare organizations can significantly improve population health outcomes, navigate the complexities of value-based care, and achieve sustainable success. Discover how you can pair a population health mission with technological tools to solve complex challenges without breaking a sweat.
