Surprising discoveries about the top 15 reasons people visit emergency rooms in colder months
Healthcare professionals brace themselves annually for a new crop of diseases that drive people to emergency departments (see: the COVID-19 pandemic), but there are also the usual suspects. Think: the flu, the common cold, and even whooping cough. Some of these require care at an ED, but in theory, others could be prevented before they escalate.
Arcadia dug deeper, and what Senior Manager of Customer Insights Dan Sweany found paints a more complicated picture. Here, we’ll delve into the discoveries the Customer Insights team made as they explored 2021 MSSP data, organizing what they found by groups of ICD-10 codes. The result is a list of the most common reasons for winter emergency room visits, and a window into what conditions a value-based care organization or provider network could target for preventive care.
How did data analysts conduct this research?
To conduct this research, Arcadia’s data experts set some helpful parameters. They studied MSSP data from November through February of 2021. Inpatient visits — where someone shows up to an ED and then stays longer for treatment or observation — were excluded from the final dataset, and COVID diagnoses were too. They also excluded other types of data sources, like commercial payer plans or options like Medicare Advantage.
MSSP represents a more defined population, whereas a wider sampling might muddy the results. Including lots of small children, for example, would naturally skew what sort of conditions arose most often.
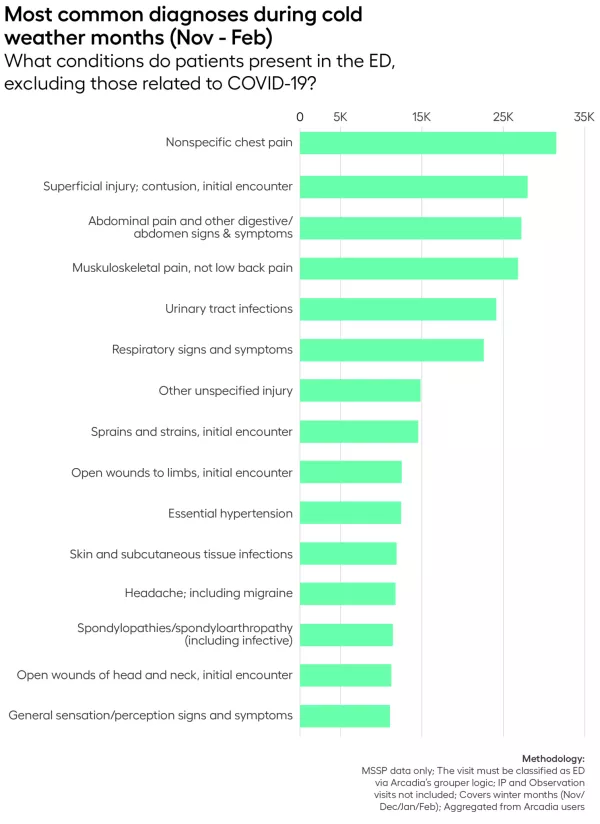
The 15 most common winter emergency department diagnoses
Each winter, emergency departments are inundated with particular diagnoses. They’re somewhat variable year by year, but data often reveals patterns, like recurrent issues providers can expect to see with every cold snap.
Arcadia’s Customer Insights team narrowed the list to the top fifteen. We’ll start at the bottom of the list, then work our way towards the most common reason people seek emergency care from November–February.
Use this list to jump to a section:
- Nonspecific chest pain
- Superficial injury; contusion, initial encounter
- Abdominal pain and other digestive or abdominal signs/symptoms
- Musculoskeletal pain (not back pain)
- Urinary tract infection
- Respiratory signs and symptoms
- Other unspecified injury
- Sprains and strains, initial encounter
- Open wounds to limbs, initial encounter
- Essential hypertension
- Skin and subcutaneous tissue infections
- Headache, including migraine
- Spondylopathies/spondyloarthropathy
- Open wounds of head and neck, initial encounter
- General sensation/perception signs and symptoms
15. General sensation/perception signs and symptoms
Most often, these sensation and perception issues are aligned with vertigo. Feeling dizzy? That could be a result of numerous different conditions, from a peripheral vestibular disorder to Ménière disease. It’s important to rule out stroke, but often, the root cause is linked to the inner ear.
14. Open wounds of head and neck, initial encounter
Yikes. If there’s an open wound in your neck or head, you probably need to be at the emergency room. It could have originated in a car accident, an altercation, or an on-the-job snafu, but in any case, sometimes these major accidents are unavoidable.
13. Spondylopathies/spondyloarthropathy
Spondylopathy is a disorder where the spine and joints can become painfully inflamed. Like arthritis, this is a chronic condition best addressed by a rheumatologist. So why are people presenting with it in an ED?
If it’s a spinal fracture or an airway restriction, obviously emergency treatment is crucial (this PDF from the Spondylitis Association of America sheds light on those risks). For general, persistent pain, patients need a regular cadence with their specialists. If organizations are looking to reduce spondylopathy codes in their EDs, helping facilitate that relationship would be a great start.
12. Headache, including migraine
Headaches run the spectrum from “drink some water and pop an ibuprofen” to “violently ill.” For the former, patients should be anywhere but an emergency room. For the latter, this article provides a checklist to help determine whether it’s worth seeking care at an ED. Additionally, there are long-term treatments available (from injectables to dietary changes) that can help keep people from reaching the point of serious illness.
11. Skin and subcutaneous tissue infections
An infection’s as unpleasant as it is time-sensitive. Once a raging infection has taken hold, medical intervention is critical.
“Tissue infections like cellulitis can get very serious very quickly, especially when combined with existing chronic conditions such as diabetes and cancer. The vast majority can and should be treated in a primary care setting, but of course that doesn’t always happen,” Sweany says.
There are a handful of ways to avoid these cases, even if some are inevitable. One step is referring patients to primary care or an infectious disease specialist, so a patient can see their doctor and say, “Hey, this looks a little strange.” Antibiotics work more quickly when the infection is less advanced. Another avenue is patient education around cleanliness and hygiene, particularly for recurrent issues.
10. Essential hypertension
Hypertension’s a common condition across the US, but it afflicts certain demographics at much higher rates. Here’s a great example of a place where SDoH data and outreach might help an accountable care organization provide better care, lessening the number of hypertension-related ED visits.
9. Open wounds to limbs, initial encounter
With many wounds, there’s no alternative to the emergency room — time’s of the essence. That said, there might be room to help patients avoid these wounds altogether.
If a value-based care network in the Pacific Northwest sees a disproportionate number of logging accidents, for example, this would give them the impetus to reach out to lumberjacks, possibly offering safety training or on-site medical visits.
8. Sprains and strains, initial encounter
When Timmy twists his ankle at the Little League game, his parents probably rush him to an ED for treatment. But think twice next time you’re sore after flag football — an urgent care clinic could be a better bet.
According to this piece from Scripps, a major driver to emergency departments is their hours of operation, which extend beyond a primary care physician’s. Urgent Care clinics pose a great alternative, providing care for non-life-threatening conditions like sprains and strains until a specialist can weigh in. It’s a great opportunity for hospitals to educate patients, particularly for ACOs or IDNs with urgent care facilities in their network.
7. Other unspecified injury
Vague? Sure. A catch-all for the many distinct reasons people seek emergency medical care? Certainly. If it’s not a sprain, a serious cut, a wound in need of stitches or antibiotics, or anything else on this list, it might go here.
6. Respiratory signs and symptoms
Maybe this year’s RSV chaos has showed up on your news feed. Either way, it’s winter sickness season, so chug some Emergen-C and wash your hands.
“It’s not surprising to see things like respiratory infections high up on the list,” Sweany says. Put simply: “It’s the winter. People get sick.”
5. Urinary tract infection
To those outside the healthcare industry, this might come as a surprise, but Sweany says it’s often highly ranked. One important factor that divides all of these diagnostic codes is urgency: does someone really need to go to the emergency room for a UTI and not, say, their primary care physician?
In many cases, healthcare networks could greatly reduce the number of UTI-related ED visits by educating the patients they serve.
“A lot of it is patient education and nature — understanding that it hurts, but the call is not to the ambulance, the call is to your doctor, or to urgent care, where it’s more expensive than a PCP setting, but less expensive than an emergency department visit,” Sweany says.
4. Musculoskeletal pain (not back pain)
These trips, Sweany says, might be avoidable. This category encompasses everything from arthritis (which is chronic, and best treated by a primary care physician and/or specialist) to repetitive stress injuries like carpal tunnel. In any case, preventing issues with ergonomic support or routine care at a doctor’s office could keep these patients healthy without the additional strain on a hospital’s ED.
3. Abdominal pain and other digestive or abdominal signs/symptoms
Here’s another category where the severity of the issue could run the gamut. These categories are groupings of related ICD-10 codes, which means “abdominal pain” could be constipation — take some fiber and stay out of the ER! — or a serious intestinal blockage. For mild pain, Mount Sinai recommends hydration and a mild diet until the discomfort passes, but watch for indications of a serious problem, which include accompanying chest, neck, or shoulder pain, prolonged illness, or bloody… we’ll just leave it there.
2. Superficial injury; contusion, initial encounter
Naturally, broad categories like “superficial injury” beg the question — what kind? And how did it happen?
“I thought that the superficial injury one was interesting in that typically, you see injuries happen more frequently over the summer months, because people are out and doing things,” Sweany says. In that regard, summer does feel riskier — there are lawns to be mowed and fireworks being shot.
Winter, though, has its fair share of risky activity, from sledding to slipping on icy stairs. This category presents an opportunity for individual health organizations to investigate the highest risks in their communities, and that might look different in Palm Beach, FL than it does in Des Moines, IA.
1. Nonspecific chest pain
Like the prevalence of respiratory illness, chest pain is a common complaint in emergency rooms, but unlike the flu, this affliction shows up year-round.
What ailment could chest pain indicate? There are so many possible reasons a patient might experience it that Arcadia’s diagnosis grouper logic was especially helpful here.
“There are thousands of ICD-10 codes, and Arcadia’s grouper classifies all those codes into categories and subcategories so that we’re able to see all the chest pain types of diagnoses without seeing, you know, 700 different cuts and 700 different variations of a single diagnosis,” Sweany says.
Some instances might be preventable, but as heart disease is the leading cause of death for men and women in the US from most backgrounds, chest pain is a valid reason to head straight to the nearest hospital.
How to reduce emergency room visits this winter
A series of data points is just that — discrete measurements, floating around in the ether. But when we string them together and view them in context, important stories can emerge. Here, the data illuminates opportunities healthcare institutions can take to become more efficient and better equipped to prevent emergency illness.
Looking to prevent unnecessary ED visits? Outreach and patient education could be the key to reducing these numbers. Check out Engage, Arcadia’s AI-powered care management tool, to learn how technology and empathy can power behavioral change.
