How to make the most of value-based care contracts
Medicare Advantage (MA) policy changes are shaping modern healthcare, and the Centers for Medicare & Medicaid Services (CMS)’s goal of enrolling 100% of Traditional Medicare beneficiaries in VBC programs by 2030 will accelerate this transformation. This shift in provider reimbursement models demands that healthcare organizations sharpen their value-based care strategies, and understand what value-based care means for their business.
Increased financial incentives for high-quality care raise a key challenge: optimizing value-based care contracts to ensure financial success. Contract optimization directly impacts the providers’ and payers’ ability to thrive under this system, influencing revenue opportunities and quality of care.
To make the most of value-based care contracts, teams across the healthcare industry must understand the full context of effective contracting, including:
- FAQs about value-based care contracts
- Core components of value-based care contracts
- Challenges of value-based contracting
- How to get the most out of value-based care contracts
- An understanding of the initial starting position (headwind/tailwind/neutral)
- A strong internal measure of model fidelity
With a thorough understanding of fundamental concepts and a leading value-based care solution, providers, payers, and beneficiaries can all thrive under this payment model.
FAQs about value-based care contracts
What are value-based care contracts?
Value-based care (VBC) contracts are contractual agreements between providers and payers that dictate reimbursement for services based on clinical performance and care outcomes. Under a VBC system, payers or government organizations like CMS compensate providers for improving the overall health and eliminating financial waste of a member population. In other words, they’re paid to get results.
How do fee-for-service and value-based contracting differ?
Value-based contracting represents a transformative shift from the traditional fee-for-service (FFS) model, in which payers reimburse providers based on the quantity of services delivered, rather than the quality and efficiency.
The main difference between the models lies in their incentives — the VBC model focuses on improved health outcomes and patient experience, but FFS has historically incentivized a high volume of procedures and services, leading to unnecessary over-utilization.
While the FFS model doesn’t hold providers accountable for patient outcomes, it’s less complex in terms of administrative burden because of its service-based billing. Still, teams across the care continuum realize benefits from VBC systems and contracts.
What are the benefits of implementing VBC contracts?
The advantages of value-based contracting are rooted in nationwide healthcare cost concerns — the United States spends more than 16% of its GDP on healthcare (at least 4% more than other nations with comparable economies), but has the highest rates of preventable deaths and the lowest life expectancy.
This spending presents an opportunity to shift the quality and cost of care from payers to providers. By incentivizing high-quality care, payers encourage providers to focus on member and patient outcomes rather than the cost of services. This makes VBC contracts beneficial to all parties across the care continuum.
- Providers: Value-based care rewards providers who achieve greater patient outcomes and reduced costs. This allows providers to prioritize care rather than meeting a quota of services. For example, providers may be rewarded for reducing costly hospitalizations by promoting preventive care to patients with chronic conditions.
- Members: An increased focus on proactive care helps beneficiaries avoid adverse health events and unnecessary medical costs. As a result, members achieve better health outcomes and are generally more satisfied with their experience.
- Payers: Payers can avoid unnecessary costs by incentivizing high-quality care. When providers help members prevent costly health events, payers can avoid having to reimburse them for unnecessary medications, hospital stays, and adverse outcomes.
Keep in mind that the division of financial responsibility and quality incentives under this model depend heavily on the type and terms of the VBC contract implemented.
What are the different types of VBC contracts?
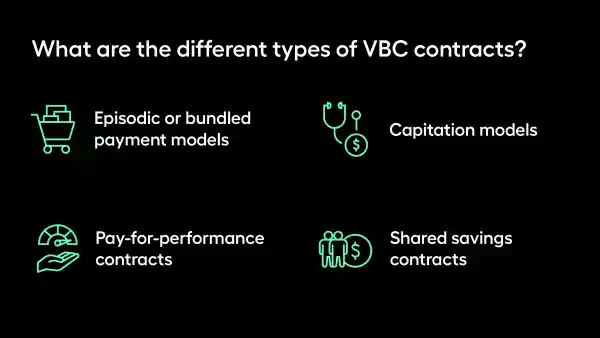
Episodic or bundled payment models
In episodic payment models (EPMs), providers assume full financial responsibility for all costs related to one specific health event, or episode of care. Providers agree to a defined cost for an episode of care, which includes all services associated with the health event.
Payments may take one of two approaches:
- Prospective, where providers are paid before the episode of care occurs
- Retrospective, where providers are paid after the episode of care through reconciliation
EPMs encourage providers to prioritize effective care coordination, as revenue under this model hinges upon the ability to increase care quality at reduced costs. Providers share any savings under this model, but they must absorb extra costs.
Capitation models
Under capitation models, payers compensate providers a fixed amount of capital per member over a set period of time. Here is how it works:
- Before the performance year begins, payers determine a fixed amount based on each beneficiary's expected care utilization and cost. Member populations with greater medical needs are generally assigned higher capitation amounts since they’ll require more care and attention to manage their illness burden.
- Providers use the capitation amount to deliver care. Similarly to the episodic model, providers may keep any extra funds if they use less than the capitation amount, but must cover excess costs if they use more.
- Payers may also establish risk pools, which set additional funds aside to cover unexpected costs. Payers withhold this money from providers until the end of the performance year and award it if the provider spends less than the capitation amount.
- Payers are not only risk adjusting, but benefit design adjusting capitation amounts to account for the different copay, coinsurance, and deductible amounts that heavily influence patient utilization.
Pay-for-performance contracts
Pay-for-performance (P4P) contracts reward providers with financial incentives for meeting specific performance benchmarks. While these contracts vary in structure, they often include a small fixed payment to help providers manage member care and award additional payments based on members’ outcomes, satisfaction, and other metrics.
The P4P model is the least risky types of VBC contracts because providers face no financial penalties for failing to save costs. Instead, this model simply rewards quality performance and withholds rewards from underperforming teams. This structure enables providers to focus more on member outcomes and care quality.
Shared savings contracts
Under shared savings contracts, payers establish a baseline budget for the cost of providers’ services, otherwise known as the total cost of care (TCOC). Then, payers compare providers’ actual TCOC to the agreed-upon benchmark and reward providers for any surplus earned.
Payers generally reward providers a percentage of any generated savings, which may be determined according to:
- Quality scores: Providers who meet or exceed performance benchmarks may receive a higher percentage of generated savings.
- Gainshare terms: Over the duration of a 3-5 year agreement, providers may begin to share in more of the value they create (and the losses).
- Credibility: some payors may set a minimum attribution requirement before they give a Provider “credit” for creating value, which makes assignability really important to focus on, in particular “addressable churn”.
Core components of value-based care contracts
At the most basic level, VBC contracts define how success will be measured and the rewards for meeting those expectations. While contracts can vary based on the health plan, member population, and other factors, value-based care contracts generally consist of several components related to quality and cost.
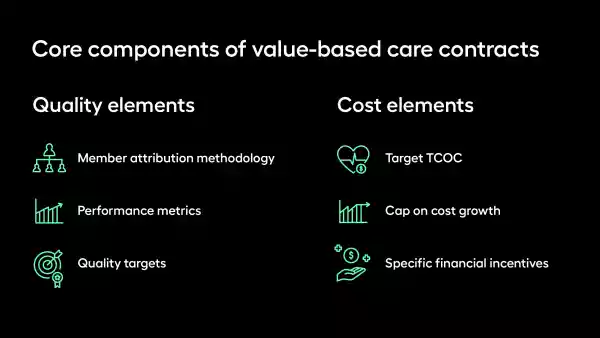
Quality elements
A significant portion of value-based contracting is negotiation (more on this later), which involves establishing the quality measures that will be used to determine efficiency and the methodologies for monitoring those metrics. This includes a few key elements:
- Member attribution methodology: For a VBC agreement to be effective, each party must agree upon a method for attributing a member’s outcomes to the provider’s efforts. This can be done prospectively (by assigning the member to a provider before receiving care) or retrospectively (basing reimbursement upon the actual care received).
- Performance metrics: The contract must define specific results that will be used to measure a provider’s performance. Metrics might include member outcomes, cost savings, reduced hospital readmissions, or other quality indicators relevant to the provider’s services.
- Quality targets: The contract must also specify the benchmarks that indicate a provider’s performance warrants reimbursement. For example, payers may reward a 30% reduction in hospital readmissions with a significant financial bonus.
Cost elements
Contract negotiations also involve setting specific financial goals, relating to both the TCOC and the financial incentives awarded for meeting the agreed-upon performance benchmarks. As such, VBC contracts typically include:
- Target TCOC: Contracts provide the financial benchmark, based on the historical TCOC and calculated on a per member per month (PMPM) basis, that a provider must aim to meet. This calculation may be adjusted for the TCOC in the region or market where the provider practices.
- Cap on cost growth: If the target TCOC is regionally comparative, contracts may also include a limit on how much that cost can increase each year (i.e., cost growth cannot exceed the regional growth rate by more than a set percentage). This cap protects payers from excessive growth in costs, but it can be unfair to providers serving members’ complex needs.
- Specific financial incentives: Because the VBC model rewards quality outcomes, contracts typically define the specific incentives providers can expect from meeting or exceeding performance targets. Contracts might also include financial penalties for underperforming providers.
Challenges of value-based contracting
Despite the many advantages of value-based contracting, health systems face several common obstacles in contract design, such as:
- Lengthy negotiation cycles: Negotiation for value-based care contracts involves many teams getting on the same page about contract terms. This process can take several months (or even quarters) to settle on information sharing, counter-proposals, and other key elements of the contract.
- Siloed and unstructured data: Even teams that easily align on contract terms can run into roadblocks when underwriting the contract with data scattered across different systems. Without a centralized data collection system, contract design quickly becomes complicated and disorganized.
- Lack of financial clarity: Participants in value-based care are responsible for various financial items provided by the payer. However, a lack of clarity around these items causes missed revenue, opportunities, or value, which is detrimental to a program’s success.
This process is especially complex for health systems that lack an in-house actuary to analyze specific contract terms. While these challenges make it difficult to implement value-based care contracts, the right solution can simplify each aspect of contract design to help address these obstacles.
How to get the most out of value-based care contracts
Arcadia’s Contract IQ makes it easier for health systems to create, manage, and negotiate value-based care contracts. Additionally, payers can use Contract IQ to model contracts and streamline negotiations and performance with providers.
With Contract IQ, you can:
- Create and collaborate on contracts: Users can create new contracts using fully customizable templates and store them in a shared library where team members can search, analyze, and edit them. Contract IQ streamlines the creation process by accepting raw contract files and using large language models (LLMs) to extract metadata.
- Enhance data sharing: Contract IQ centralizes contract management, providing a single platform for all team members to collaborate on each aspect of the contract creation process. Easily track performance metrics and quality goals to develop contract terms that align with care costs.
- Unlock financial clarity: Real-time data modeling in Contract IQ helps forecast financial outcomes of different contract scenarios. With these insights, health systems can optimize contract terms, maximize value, and course correct any pattern of expense that differs from their forecast.
- Improve negotiation power: By offering a clearer view of providers’ savings in the context of specific contract terms, Contract IQ empowers health systems to understand the opportunities and have more productive conversations with payers when negotiating. As a result, providers can develop data-backed, performance-based proposals to make each contract more beneficial for all parties.
- Actuarial forecasting: Our product offers a view of in year performance across all TCOC contract types, using our scalable solution to estimate what expenditures will look like based on actuarial modeling.
Leverage technology to streamline value-based care contracts and beyond
Value-based contracting is a lengthy, complex process, and it’s only one part of success under this payment model. Providers need high-performing networks and contracts that align financial incentives with care quality, on top of data-driven insights and care plans to tap into the benefits of value-based care.
Arcadia’s health data platform covers all of these bases and much more. Our robust solution is dedicated to transforming data into actionable insights for ACOs, health systems, and payers alike. By investing in the right tools, your organization can optimize its value-based care strategy from all angles.
