10 leading chronic care management software picks of 2025
According to research from the CDC, approximately 129 million (nearly 40%) of people in the United States have at least one major chronic disease. Five of the top 10 leading causes of death in the U.S. are (or are strongly associated with) preventable and treatable chronic diseases, underscoring the immense need for effective chronic care management from health systems.
Efforts to manage chronic conditions require participation from patients, providers, and payers. This involves timely interventions, lifestyle changes, continuous symptom monitoring, and other elaborate care plans. As such, chronic care management software has become an increasingly important tool for health systems looking to optimize workflows while delivering highly personalized, data-driven care to patients with long-term conditions.
This article explores the capabilities and impact of implementing such software and reviews the top chronic care management companies that offer relevant solutions.
An overview of chronic care management software
What is chronic care management?
Chronic care management often refers to the value-based Medicare services that deliver support and high-quality care for individuals with two or more chronic conditions. However, providers can apply this approach to all patients facing at least one chronic condition to enhance the quality of care across the board.
To put it plainly, chronic care management is the process of monitoring patients’ chronic conditions and optimizing interventions, such as regular appointments and medication adherence, to improve overall outcomes.
Chronic care management programs are the structured approaches providers take to deliver this level of care, encompassing patient monitoring, education, and ongoing support to help individuals learn to live with their conditions and avoid adverse health events. Medicare-based chronic care management programs are easily reimbursed. However, there are other ways to get reimbursed for this service, meaning providers can still implement similar programs to support patients who don’t qualify.
What is chronic care management software?
Chronic care management software is a solution that helps healthcare providers manage the care of patients with chronic conditions to improve their quality of life and outcomes. Such solutions enable providers to address barriers to effective chronic care management, including inadequate infrastructure for health information exchange with other providers and limited electronic health record (EHR) capabilities for documenting and updating care plans.
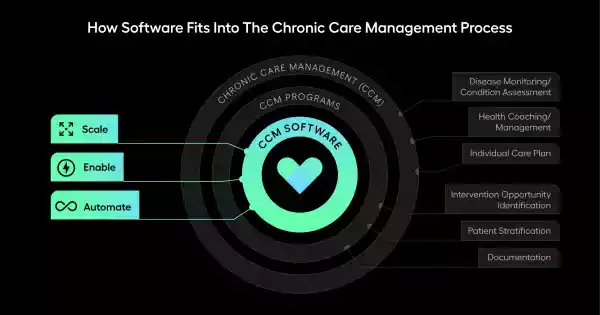
Research suggests that data plays a critical role in identifying and monitoring chronic conditions. Considering technology’s significance in efficient healthcare data management, it’s clear that software is a vital tool in delivering high-quality care to patients with chronic conditions.
How does chronic care management software benefit healthcare systems?
With an understanding of this software’s capabilities and its role in the greater healthcare landscape, it’s easy to see the vast benefits of implementation for parties across the care continuum:
Benefits for patients. When providers implement chronic care management software, patients experience more personalized treatment plans, reduced medical emergencies, and overall better outcomes. They also become more involved in their care and gain a greater understanding of their conditions.
Benefits for providers. Chronic care management solutions equip providers with centralized access to patient data, streamlined communication, enhanced care coordination, and other tools that help them make informed decisions.
Benefits for payers. Early interventions, increased member satisfaction, and improved outcomes driven by powerful software yield lower costs for payers. Additionally, care management tools provide aggregated care data to help payers gain better population health insights.
Key features of chronic care management solutions
When assessing available tools to facilitate better chronic care management, providers should ensure these solutions offer all of the capabilities they need. Key functionalities include:
Patient data aggregation. Effective solutions integrate patient data from various sources to help providers identify patients with high care management needs and update care plans accordingly.
Care coordination. Health teams can collaborate by pushing notes back to the patient’s electronic health record through care management software.
Patient engagement. Providers equip patients to take an active role in their chronic care management using engagement tools in their software that facilitate ongoing patient-provider interactions.
1. Arcadia: Leading chronic care management software provider
Data aggregation and analytics are critical for taking informed steps in the care journey, especially when embarking on a long-term journey toward chronic care management. That’s why Arcadia’s leading analytics platform is the top solution on the market for chronic care management.
Arcadia empowers healthcare organizations to create robust, configurable care management programs through a series of automated workflow tools. These features enable providers to identify risk factors and address health concerns early, allocate resources efficiently by estimating costs and potential savings, and measure impact to refine processes over time.
Specifically, Arcadia’s care management module offers the following applications:
Analytics dashboards. Uncover deep and actionable insights to empower data-driven decisions through self-service dashboards.
Patient engagement tools. Identify care gaps and automate outreach for targeted communications and scaled care management programs.
Social determinants of health (SDoH) data. Identify populations most in need of care through a unified registry of patient-level insights.
Patient stratification capabilities. Build a comprehensive list of patients with gaps or access a holistic view of your population so you can reach out as needed.
These tools yield impressive results for organizations that partner with Arcadia:
A Northeast ACO had a 41.5% reduction in ED visits for COPD patients
A multi-state ACO reduced treat-and-release ED visits by 69,000
Another Northeast ACO served 3x more patients with the same care management team
Arcadia’s solution supports health organizations with chronic condition management, transitional care management programs, nonclinical care coordination, and more.
2. CareJourney: Supports care coordination
Acquired by Arcadia in 2024, CareJourney combines clinically relevant healthcare data with AI-powered analytics and insights. This tool derives market-leading analytics from Medicare, Medicaid, Medicare Advantage, and Commercial claims data across more than 300 million patients and over 2 million providers nationwide.
CareJourney allows healthcare organizations to take a closer look at patient data, surfacing insights about care patterns and outcomes. As a result, various health teams can coordinate care more efficiently and make informed decisions that improve long-term health.
The combination of Arcadia and CareJourney has already driven significant results, helping Accountable Care Organizations (ACOs) deliver better patient outcomes and lower healthcare costs. On average, ACOs supported by Arcadia and CareJourney achieved 1.5x more savings compared to other ACOs nationally and generated $815 million in total savings in performance year 2023.
3. Vim: Powers integrations
Vim is a middleware platform and clinical workflow integration technology that incorporates essential data, insights, and applications into existing EHR workflows. Payers, providers, ACOs, and other teams across the care continuum can use this tool to:
Streamline referrals
Optimize risk adjustment
Automate chart retrieval
Expand patient insights
Vim’s integration capabilities fold care opportunities into clinical workflows, allowing providers to implement timely and data-driven chronic care interventions.
4. J2 Interactive: Drives interoperability
While J2 Interactive isn’t a traditional care management tool, this software development and IT consulting firm has twice been ranked #1 for Technical Services in the annual Best in KLAS survey. Their team specializes in customized solutions for teams across the care continuum, guiding healthcare organizations through complex data and interoperability projects such as:
Extracting data from EHRs
Integrating and implementing technology platforms
Data enrichment and management that supports improved data connectivity, completeness, and accuracy
Considering the impact of complete and integrated data on chronic care management, J2 Interactive’s services are critical for more accurate tracking, better care coordination, and improved patient outcomes.
5. HealthHelper: Closes care gaps
Panel management involves proactively addressing your patient population’s health needs, including implementing targeted interventions and improving patient outcomes. Primary care providers need effective panel management to drive proactive patient care, which ultimately supports chronic care management.
HealthHelper’s platform leverages robust data to automate, streamline, and scale panel management workflows. Their technology-enabled service provides:
Panel analytics
Attribution cleanup
Care campaigns
Patient scheduling
Care gap closure
Detailed reporting
By optimizing panel management, HealthHelper ensures that patients facing chronic conditions receive timely follow-up, preventive care, and personalized outreach.
7. N1 Health: Delivers predictive insights
N1 Health is an AI-driven platform that generates meaningful predictions concerning patient outreach and interventions. From identifying the right audience to informing data-driven interventions, this platform enables better health outcomes, especially for those with chronic conditions.
The ability to anticipate patients’ needs and intervene early is critical for effective chronic care management. A proactive approach improves medication adherence, reduces hospitalizations, and fosters consistent engagement for better outcomes, which N1 Health delivers via predictive analytics.
8. Atropos Health: Provides real-world evidence
Atropos Health’s focus on high-quality evidence is essential for managing complex, long-term conditions. This platform uses real-world data (RWD) to enhance evidence-based decision-making, which has been shown to elevate clinical outcomes, accelerate research, and drive operational efficiency.
These capabilities enable healthcare organizations to:
Accelerate time to treatment
Inform rapid drug discovery
Reduce the cost of care
Expedite research from months to minutes
Address car variation
Augment staff and efficiency
With personalized evidence for every clinical decision and research inquiry, Atropos Health supports informed decisions about chronic disease treatment paths.
9. Athenahealth: Offers general healthcare management tools
Athenahealth offers care management tools to help healthcare organizations coordinate care and engage patients. While they primarily serve providers, the tool also allows providers and payers to exchange information for simplified administrative tasks.
While Athenahealth’s offerings are centered around more generic functionalities, the platform still supports the foundational elements for effectively managing chronic conditions, such as patient tracking and timely updates.
10. HELIOS Care Management: Features various tiers
HELIOS by VirtualHealth offers a care management tool purpose-built for value-based care, featuring user-friendly point-and-click tools and different configuration levels based on your team’s management needs. While not a dedicated chronic care management company, this provider’s tools still include helpful capabilities for addressing long-term conditions.
Through built-in telehealth tools, mobile apps for care teams and members, and 100+ data integrations, HELIOS equips providers with data-driven insights to engage patients.
How to choose the right chronic care management solution
To choose the right solution, healthcare organizations must first evaluate their needs in regard to managing patients with chronic conditions. Then, they’ll be prepared to:
Identify must-have software features, such as analytics dashboards or risk assessment capabilities
Flag deal breakers, like an interface that makes it difficult to visualize long-term patient data
Review case studies to determine the provider’s success with similar organizations
Consider ease of use and scalability, selecting a tool that the health team can work with comfortably
Once you’ve selected your top contenders, request a demonstration of each solution to experience its features firsthand. This demonstration will also allow you to interact with the provider and gauge the level of support you can expect to receive from their team.
Leverage Arcadia’s chronic care management software for greater results
The right solution can make the difference between successful chronic condition management and a lacking program. As an award-winning platform for its robust analytics capabilities, Arcadia is the number one solution for improving the quality of care for patients with chronic conditions. Will your healthcare organization be the next to benefit from it?










6. Socially Determined: Surfaces SDoH insights
Studies show that an individual’s social context has significant implications for their experiences with chronic conditions, including their risk of exposure, degree of susceptibility, and the course and outcome of the disease.
Socially Determined’s platform delivers social risk data and analytics to help healthcare organizations understand the impact of social determinants of health (SDoH) and social risk factors on the populations they serve. Powered by a robust data supply chain, this solution delivers insights that provide complete visibility into a patient or health plan member’s social risk.
With this platform, organizations can drive strategic programs that deliver measurable improvement in health outcomes at scale.