Unwinding the public health emergency and tackling the redetermination crisis

The COVID-19 public health emergency comes to an end
The Public Health Emergency (PHE) for COVID-19 is set to expire on May 11, 2023. As our healthcare system readjusts to new norms and uncertain realities, it's helpful to look back at how we navigated this trying time. We invite you to explore two data visualizations that capture what those early days of the pandemic were like: (1) 1M COVID-19 cases and their symptomatic journey and (2) COVID-19’s impact on service lines.
ARCADIAN INSIGHTS
Anna Basevich on unwinding the public health crisis, and how we can help Medicaid beneficiaries retain their benefits
The mental math to sign up for healthcare coverage is complicated. Whether you’re evaluating Medicare Advantage plans for the first time, or you’re a full-time employee of a healthcare technology company (like me) going through open enrollment forms, it can be a challenging process – and that’s just those of us who don’t have to demonstrate our income to sign up for and retain coverage.
For millions of Americans, the PHE for COVID-19 made things a bit easier. States were required to implement continuous coverage, which paused redetermination — the process of re-submitting the paperwork necessary to qualify for Medicaid coverage. And so for the past few years, beneficiaries and their support systems (MCPs, health systems, social services) fell out of practice with this process. Redetermination is about to start up again, which is going to cause an added burden on our country’s healthcare system and could cause millions of Americans to lose coverage if they fail to navigate the complex process.
Preventative care, chronic disease management, and access to emergency services — all foundations of success in population health management — are at jeopardy. While states are required to send multiple notices to beneficiaries before terminating Medicaid coverage, the Medicaid population has not been in the habit of responding to these letters for the past three years. Many may have never had to go through redetermination if they began receiving coverage due to changing circumstances during the pandemic. Others may not have the financial literacy to pull together the proper documentation, or they may have language barriers with completing the forms. Those lacking stable housing may not even receive mail at the address on file. Given the barriers, helping Medicaid beneficiaries retain coverage requires an all-hands on deck mentality.
As we unwind the PHE over the next few months, how can you help your Medicaid population keep their coverage and navigate redetermination? Last year, I wrote an article for MedCity News detailing a 3-step plan that providers and payers could follow to support Medicaid beneficiaries in the process. That plan is still valid today: (1) Inform Medicaid patients of the need to re-enroll, (2) Strengthen your relationship with the beneficiary, and (3) Ensure outreach campaigns are omnichannel and multilingual, accounting for barriers to redetermination the same way that we account for barriers to care in addressing care gaps. Leverage your trust with patients, help them tap into community resources to successfully navigate redetermination, and cater to them in the languages and channels which they use to communicate.
Technology plays a crucial role in successful unwinding. At Arcadia, we’re already having conversations with customers to formulate a plan. They’re using Arcadia Analytics to build Medicaid patient lists, identify renewal dates, contact preferences, and languages spoken, and automate outreach with templated messages. Many organizations are getting messaging out that says, “Hey, it’s not too early to start thinking about Medicaid coverage” or “Your coverage is contingent on getting documentation together.” We recommend starting this outreach at least three months before a patient’s renewal date, leveraging multiple methods of communication, because it often takes multiple touch points to build urgency and drive action.
For better or worse, unwinding is here. This could create a huge burden on our healthcare system, but it doesn’t have to. With the proper application of technology, we can keep those who need coverage covered, while preventing further burnout amongst clinical staff resources. I encourage you to make a plan today and reach out if you need support.
Stay well,
Anna Basevich
VP Enterprise Partnerships
Arcadia
PRODUCT SPOTLIGHT
Patient Registry: Build cohorts, stratify patients, and close gaps quickly
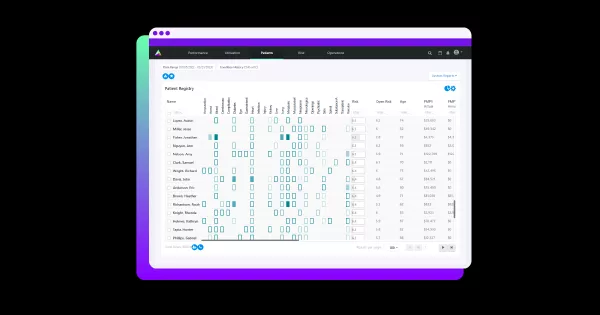
Arcadia Patient Registry allows health systems and their providers to build a comprehensive list of patients with gaps, instantly reach out via text-message, and generate custom reports. Zero in on individual patients, or get a comprehensive view of your population.
NEWS YOU CAN USE
Let’s put data to work to solve emerging challenges in healthcare
15M people, including 6M children, could lose their Medicaid benefits. For the past few years, beneficiaries did not have to re-enroll for these benefits. Now that the public health emergency caused by COVID is ending, states fear that unwinding the expanded social safety net could prove messy. [POLITICO]
Last year Medicaid enrollment grew to 91.3 million, an increase of more than 28.5%. There are many factors that might explain this increase, including the continuous enrollment provision included in the Families First Coronavirus Response Act (FFCRA), but that is ending on April 1, 2023. [KFF.ORG]
Black individuals account for 14 percent of people expected to lose eligibility. Other groups disproportionately affected by the end of PHE include young adults, Latino individuals, and low-income households. [HEALTH PAYER INTELLIGENCE]
JOIN THE CONVERSATION
Tune In: Redetermination is looming — what healthcare organizations can do to help
Every month, we get a pulse on the most important topics in healthcare and data.
The public health emergency caused by COVID-19 is officially ending, meaning states must restart redetermination. Join Arcadians Jessi Cardello and Josh Cabana as they explore how health systems, provider networks, and payers can help their members and patients keep the coverage they need. Tune in live, or subscribe to stay updated on future episodes and on-demand recordings.
