How to navigate performance improvement in healthcare
Whether operating under value-based care (VBC) contracts or traditional fee-for-service (FFS) models, improving care quality while managing costs is a major priority across the healthcare sector. As such, health systems must analyze and optimize their current performance to optimize efficiency, improve outcomes, and maintain financial sustainability.
This article explores the importance of performance improvement in healthcare and the data-driven strategies your organization can implement to analyze and optimize its performance.
FAQs about performance improvement in healthcare

What is performance improvement in healthcare?
Performance improvement in healthcare is a continuous process of making strategic efforts to enhance care quality and efficiency. This process involves analyzing data to identify areas for improvement, implementing necessary changes, and monitoring the impact of those adjustments over time.
The end goal of performance improvement is to drive better patient/health outcomes, increase revenue, and reduce costs, bringing benefits to stakeholders across the care continuum.
What are the benefits of healthcare performance improvement?
From health systems and payers to independent practices and provider networks, every stakeholder in the health industry stands to benefit from performance improvement. Effective performance improvement strategies strengthen a health system’s sustainability, offering benefits to patients, payers, and providers alike.
Improved patient outcomes
By enhancing care quality and efficiency, patients experience improved outcomes through:
Data-driven decision making. With a heightened focus on performance improvement, providers can continuously analyze data to assess patients’ health statuses. Data insights enable providers to make informed decisions regarding care plans and even predict future health events for proactive interventions.
Improved care coordination. As part of their performance improvement efforts, providers aim to enhance care quality, which relies on using a holistic view of patient health to identify gaps in care and deliver timely and proactive healthcare interventions. Complete, real-time patient data enables consistent and efficient treatment across different departments.
Delivering whole-person care. Improving outcomes doesn’t mean addressing just one medical need; rather, it involves treating patients holistically, including both health needs and nonmedical factors impacting health. By understanding and supporting the full context of a person’s life (e.g., transportation, trust, health literacy), providers can drive better overall outcomes.
Cost savings
Performance improvement drives significant cost savings by:
Enhancing physician performance. Modern healthcare focuses on fostering accountability for a broad set of outcomes rather than meeting isolated quality metrics. Using integrated data, providers can better understand performance gaps where providers fall short. This innately reduces healthcare costs by supporting stronger diagnoses and management.
Optimizing resource utilization. Aligning care decisions with patient needs ensures that resources are directly matched to outcome improvement. This includes avoiding unnecessary hospital or emergency visits through proactive risk management and choosing more cost-effective care settings (e.g., outpatient instead of inpatient) without sacrificing quality.
Aligning with value-based care models. Under value-based care (VBC) contracts, providers receive financial incentives for delivering high-quality, cost-effective care. By evaluating their performance, providers can implement cost-saving behaviors that benefit patients and health teams.
Operational efficiency
By definition, performance improvement systematically refines healthcare processes to improve efficiency. The specific process improvements depend heavily upon the healthcare organization, but may include:
Streamlining patient flow. Providers may address opportunities for improvement in patient flow, such as standardizing admissions protocols or accelerating diagnostic testing. Optimizing each step of the patient experience (i.e., admissions, diagnostics, and discharge) improves patient satisfaction and overall care delivery.
Reducing wasted time, supplies, and other resources. Health teams can address hidden waste, like redundant documentation processes or overuse of expensive supplies, to ensure the right resources are available at the right time. Eliminating these inefficiencies helps contain costs and improve outcomes.
Improving communication and coordination. Breaking down silos between departments through centralized EHRs, secure messaging, and other tools enables shared decision-making. This way, providers, payers, and other teams across the care continuum can collaborate in real time to ensure patients receive coordinated, informed care.
Minimizing administrative burden through automation. By deploying AI-driven automation tools, health teams can streamline routine workflows like patient communication and chart summarization. This helps to cut costs, reduce burnout, and allow staff to focus on patient care.
The framework for performance improvement in healthcare
The healthcare performance improvement process is cyclical, consisting of three key systems:
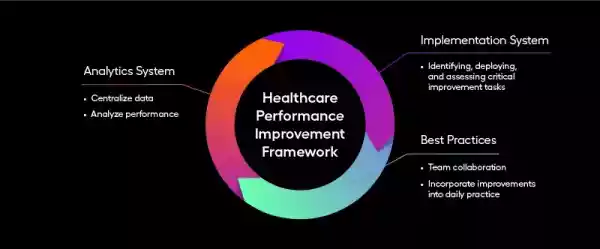
Analytics system. Healthcare organizations must centralize data from various sources to accurately analyze their performance.
Implementation system. Different teams across health systems take ownership of identifying, deploying, and assessing critical improvement tasks.
Best practices. Various teams must work together to incorporate improvements into daily practice.
Steps to implement a healthcare performance improvement program
The most important aspect of performance improvement in healthcare is continuity. Effective and sustainable improvement requires ongoing evaluation and adjustment, meaning healthcare organizations must adopt a program for assessing performance and making changes as needed by following the steps below.

1. Leverage analytics software to identify improvement opportunities.
Whether you're a provider managing population health or a payer evaluating network performance and utilization patterns, analytics platforms surface actionable data from various sources to help health systems assess and improve their performance.
Software is critical for identifying improvement opportunities, as it streamlines and automates the analytics process. Healthcare organizations can use software to uncover performance patterns, predict future challenges, and track the impact of their improvements over time. Additionally, analytics platforms present data in easily digestible reports and dashboards, allowing health teams to assess and share performance insights.
Additionally, modern analytics platforms increasingly integrate AI to enhance insights. AI leverages natural language processing to extract meaning from clinical notes and machine learning to forecast outcomes, accelerating the performance improvement cycle.
Arcadia offers two solutions that equip organizations to analyze their data and compare performance to industry standards:
Arcadia Vista Push. As a new component of Arcadia’s Vista analytics dashboard, this solution enables health analysts to create and distribute performance reports. PDF reporting enables stakeholders to quickly receive and leverage data-driven insights for broader adoption of new initiatives.
Enhanced Benchmarks. Powered by CareJourney’s market intelligence and VBC performance analytics, along with Arcadia’s de-identified benchmarks sample, this solution measures cost, utilization, risk, and quality KPIs to track performance and compare it against competing organizations. With these actionable insights, organizations can discover opportunities to boost performance.
Accountable Care Organizations (ACOs) using the combination of Arcadia and CareJourney (acquired by Arcadia in June 2024) achieved 1.5x more savings compared to other ACOs nationally. They also demonstrated notable quality improvements through preventive care, achieving higher screening rates for both colorectal and breast cancer and higher influenza immunization rates than other ACOs.
2. Prioritize improvement projects
Equipped with data-driven insights into their performance, health organizations must determine the highest-priority improvement opportunities by next assessing organizational readiness.
Organizational readiness refers to health teams’ willingness to accept change and any implications those changes may hold for clinical staff. Readiness is especially critical among the following teams:
Executive leadership
Department heads
Frontline staff
After confirming organizational readiness, align improvement projects with strategic objectives. For example, an organization focusing on population health management (PHM) should prioritize improvements that enhance care coordination or chronic disease management.
Scoring frameworks can help organizations determine which improvement initiatives to prioritize by ranking tasks according to their expected impact on critical areas of operation. Using the example above, an organization focused on PHM might rank implementing remote patient monitoring devices more highly than an initiative to reduce paper use by digitizing forms.
3. Establish teams to lead necessary changes.
Healthcare organizations must have dedicated teams in place to carry out high-priority improvement processes. Multidisciplinary teams are most effective, blending the expertise of professionals across the care continuum to define and monitor the most impactful improvements.
Clarify each team’s responsibilities, such as:
Process redesign, which involves assessing goals, properly allocating resources, and designing optimized processes
Communication and training, which involves leading the implementation process by informing staff of changes and ensuring a smooth workflow adoption
Implementing improvements, which involves directly putting new processes into action and reporting any feedback to project leaders
4. Monitor performance and calculate ROI.
After putting performance changes into motion, organizations must implement a system for ongoing measurement to sustain improvement efforts. Leverage dashboards to keep stakeholders informed about progress and hold teams accountable for adhering to necessary changes.
By leveraging performance data from before and after improvements were implemented, as well as financial data showing the cost of implementing changes, organizations can also measure the ROI of their healthcare performance improvement programs.
5. Share proven best practices across teams (and across organizations).
As healthcare organizations implement improvements, it’s critical to monitor and document successes. Some initiatives will be more impactful than others, enabling health teams to identify repeatable practices.
For example, let’s say a healthcare organization launches an initiative to reduce hospital readmissions for heart failure patients. The improvement effort may include:
Enhanced coordination with primary care providers (PCPs)
Scheduled follow-up calls after discharge
Patient education on medication adherence
If the organization monitors the initiative’s impact and observes a 15% reduction in readmissions, the health team may share their results and recommend these best practices to other departments managing chronic conditions.
Furthermore, sharing successful strategies internally is just the beginning. There’s significant value in sharing learning across health systems, which is where a connected analytics provider like Arcadia becomes a crucial resource.
Arcadia draws from a diverse network of healthcare organizations to identify scalable strategies that drive results. The goal: empowering industry leaders to benefit from collective experience and innovation. With data to back up the impact of successful performance, organizations can make the case for standardized guidelines that drive improvement across the board.
Start the performance improvement cycle with robust analytics
Establishing a system for performance improvement in healthcare starts with having access to comprehensive data. Your organization can implement sustainable improvement processes when your efforts are fueled by actionable insights and modern analytics.
In addition to providing cutting-edge analytics, Arcadia helps organizations like yours benefit from the collective intelligence of a broader network. Explore Arcadia’s solution today to discover an analytics tool that drives successful performance.
